Autoimmune Disease: A Functional Medicine Guide To Symptoms, Causes + Natural Treatments

Autoimmunity is a condition in which the immune system mistakenly over-reacts to the body’s own tissues, attempting to destroy them with inflammatory cells. The immune system is, of course, meant to protect against viruses and bacteria, so why would it suddenly mistake the body for an enemy?
Actually, there is nothing sudden about it. Many people are experiencing low-grade autoimmune reactivity years before they have suffered enough tissue damage to warrant a formal diagnosis by a conventional medicine practitioner. And it’s a major problem.
Article continues below
Make Your Life a Cleanse
SUBSCRIBER-ONLY GUIDES FOR GUT HEALTH, VIBRANT ENERGY, HEALTHY FOOD & CLEAN ALCOHOL
Get FREE access to these + giveaways, recipes, & discount codes in personal emails from Dr. Will Cole.
Research (1) from the medical journal Nature estimates that about 25 percent of us have some sort of dysfunction of the immune system,and according to the American Autoimmune-Related Diseases Association, 50 million Americans have a diagnosable autoimmune disease. Meanwhile, millions more have autoimmune spectrum problems with no explanation for their symptoms.
What is causing the rise of autoimmune conditions?
Researchers aren’t sure yet what causes autoimmune disease, but the primary theories include a genetic weakness being triggered by an immune system response to toxins; food proteins like gluten and casein leaking into the bloodstream through a compromised gut lining; or chronic viral, bacterial, yeast, or parasite infections. All of these involve out-of-control inflammation which is an immune system trigger. This inflammatory-immune response can both cause and increase intestinal permeability or leaky gut syndrome, (2) further perpetuating the inflammatory-immune cycle.
Is Autoimmune Disease Caused By Genetics Or Lifestyle?
The old view of genetics was that it was an immutable force and that if your family had a certain health problem, it would be just a matter of time before you got the same disease, unless you were very lucky. Today, we know it isn’t that simple. The field of epigenetics has explored and demonstrated that environmental factors influence DNA expression. In other words, genetics can give you the tendency to develop an autoimmune disease, but it is your lifestyle choices and your environment that determine whether those particular genes get switched on or off. In other words, our exposures may largely determine our genetic expression and the strength or weakness of our immune system.
- One Stanford study, (3) published in 2015, looked at genetic and lifestyle health factors in 210 healthy twins, both identical and fraternal. What they found was remarkable: 58% of the immune system was almost completely determined by environmental and lifestyle factors, and 19% of the immune system was largely influenced by environmental and lifestyle factors.
This is great news because it means 77% of the immune system is determined by things we can control.
The Influence Of Chemicals, Processed Foods, and Environmental Toxins
In the past 100 years, even in just the last few decades, there has been a disturbing increase in production of and exposure to chemicals, processed foods, and environmental toxins, and the fact is that our genes are struggling to keep up.
Take the effect of fast food on your Th17 cells, for example. Their purpose is to fight bacteria and fungi, but their overreaction has been linked (4) to autoimmune disease. Researchers found that a high-salt diet negatively affected Th17 cell reactions and increased autoimmune problems. Our fast food society is filled with salt levels far beyond what anyone would get eating a natural diet. This is just one of the many triggers that can cause an inflammatory autoimmune response in genetically susceptible individuals.
This is where functional medicine is a huge player. By looking at root cause triggers and using natural tools of diet and lifestyle, you can learn what your body needs to calm your over-reactive autoimmune responses, coaxing them into remission – no matter what your genes say.
Are you on the autoimmune spectrum?
The sad reality is that in most traditional medical practices, the immune system has to destroy a significant amount of tissue to be officially diagnosed. For example, there has to be 90 percent destruction (5) of the adrenal glands to be diagnosed with Addison’s disease, or severe destruction of the neurological and digestive systems to be diagnosed with multiple sclerosis (MS) and celiac disease, respectively.
In a traditional medical setting, a diagnosis won’t come until the end stages of autoimmune conditions when it may be too late to treat or reverse it. I believe in detecting and treating autoimmune disease inflammation before it does too much unnecessary damage.
This is why I look at autoimmunity as a spectrum. You can be on the low end, with some reactivity, or in the middle, with significant symptoms that are still not conventionally diagnosable, or at the end stage, when symptoms are so intense that a doctor finally says, “Yep, you have (insert disease here.)” That’s why it’s important to consider not only how to treat or reverse autoimmune disease, but how to prevent autoimmune disease from progressing as well.
Three main stages of the autoimmune spectrum:
- Silent Autoimmunity: There are positive antibody labs but no noticeable symptoms. Your doctor will likely tell you that you are probably fine, or to come back next year and re-test.
- Autoimmune Reactivity: There are positive antibody labs and symptoms, but still not enough to warrant a formal diagnosis.
- Autoimmune Disease: There’s enough body destruction to be diagnosed.
Among my patients, I find that quite a few of them are at Stage 2. They clearly know something is off but don’t have significant enough markers for traditional medical providers to give a diagnosis. I believe everyone on this spectrum deserves to feel better as soon as possible, and they can.
How To Spot Autoimmune Disease Early
Some early symptoms of autoimmune reactivity include achy muscles and joints and fatigue. I’ve also written in the past about how some cases of unexplained depression could be due to autoimmune reactivity of the brain.
Early detection of an autoimmune disease before extensive damage, could give you a sort of grace period in which to address the issue, stop the progression, and in some cases reverse the autoimmune spectrum symptoms. Start the autoimmune disease prevention process with a complete set of functional medicine labs to detect early signs of autoimmunity. Some research (6) suggests that antibodies can show up on labs several years before the diagnosis of many autoimmune diseases.
One lab I typically run on patients is what’s referred to as predictive autoimmunity, which allows us to see whether there is any abnormal immune response against many parts of the body. Some of the more common antibodies we find are:
- Stomach: Parietal cell antigens, which are associated with gastric autoimmunity
- Thyroid: Thyroid peroxidase antigens, which are associated with Hashimoto’s disease
- Brain: Synapsin antigens, which are associated with inhibited neurotransmitter release
- Adrenals: 21 hydroxylase (adrenal cortex) antigens, which are associated with autoimmune endocrine disorders
- Gut: Tropomyosin antigens, which are associated with inflammatory bowel disease
- Joints: Arthritic peptide antigens, which are associated with rheumatoid arthritis.
This simple blood test may be beneficial for someone who:
- Has unexplained symptoms but “normal” labs
- Has been diagnosed with gluten intolerance
- Has leaky gut syndrome
- Has already been diagnosed with an autoimmune disease
To be clear, functional labs like this are not used to diagnose autoimmune diseases, which is still done in the mainstream medical setting. We use labs like this to investigate underlying factors and tailor a health program to improve these issues, based on where the antibodies are.
Can you prevent autoimmune disease?
While there’s no general cure or vaccine against autoimmune disease, there are several ways you can support your body’s autoimmune response to lessen the likelihood and intensity of an autoimmune condition. We will explore some triggers to avoid, as well as supplements, foods, and lifestyle tips you can implement to support a healthy immune function. Of course, following the tips above will help with early detection in hopes of preventing any aggressive progression of an autoimmune disease that has already begun affecting your body.
Let’s dive into some of the ways you can support your body whether you are aiming to prevent or reverse autoimmune disease symptoms.
13 Surprising Triggers Of Autoimmune Conditions
I’ve already covered the multifaceted reasons for the autoimmune explosion we are seeing. Apart from those all-encompassing influences though, what triggers autoimmune disease in daily life? Let’s look at what some of these top triggers are.
Eating A Modern Diet
As mentioned before, our food culture has changed drastically in a relatively short period of time with the development of human agriculture and the onslaught of manufactured food and food chemicals. Human genes haven’t yet had the chance to adapt to these extreme changes, and this mismatch between modern food and ancient human biochemistry has, according to many experts, significantly contributed to the rise of autoimmune disease.
For example, humans eat far more grains than they ever did pre-agriculturally, and we know there is a clear link between grains and autoimmune conditions. Getting the proper food intolerance diagnostic labs done can be the first step for many to regain their health. Until you know what you personally are reactive to, you cannot know for sure what foods to avoid to cultivate health. These are the most common culprits I see:
Gluten - Even if you don’t have celiac
The infamous “G” word is a protein that’s found in wheat, barley, spelt, rye, and other grains, and is scientifically linked to an increased risk of autoimmunity. Many people and their doctors believe you have to have celiac disease to be gluten intolerant. When their labs for celiac come back negative, they are told that avoiding gluten is unnecessary. This antiquated misinformation keeps many people struggling with an autoimmune condition, feeling unnecessarily sick.
For many of my autoimmune patients, it doesn’t have to be a piece of bread or pasta to cause damage either. Foods cross-contaminated with gluten can be like gasoline on a fire for many people with autoimmune conditions. If you are suffering, try eliminating gluten for a good 90 days and pay attention to whether your symptoms get any better.
Gluten-free grains
On the other hand, many people with autoimmune problems already avoid gluten, but still consume non-gluten grain foods like corn, oats, and rice. As well-intentioned as that may be, these grains can be just as damaging as gluten, for people who are sensitive to them (and this is common with people prone to autoimmune issues).
The reason is that the proteins in these grains are very similar to gluten, and an overactive immune system may mistake them for gluten anyway and begin an attack. Just as with gluten sensitivities, symptoms do not have to be gastrointestinal in nature. A flare-up of any autoimmune symptom can occur with exposure to grains. Running immunological blood tests or trying to go grain-free can help detect or rule out this trigger.
Quinoa
A favorite in the health community, so-called pseudo-grains like quinoa are high in proteins called saponins, and these can be inflammatory and damaging to the gut lining, causing an immune response in the body. Soaking and rinsing quinoa can reduce the gut-damaging effect, but for many with serious autoimmune conditions this is not enough and avoiding quinoa altogether is a more effective strategy to quell this inflammation and symptom response.
Sugar
It should be no surprise that sugar is on this list, but I’m not just talking about the stereotypical junk food. There are many popular “healthy” junk foods that are not good for autoimmune conditions, even if they are labeled as healthy, organic, or natural.
Terms like “organic turbinado sugar” or “agave nectar” on a food label may sound less insidious than “white sugar,” but to the immune system, it’s all sugar. Try using less sweeteners and added sugars all around for better health.
Chocolate
This yummy and frankly antioxidant-rich food can be heart-healthy for some (in small, low-sugar amounts) but can cause a lot of damage to someone living with an autoimmune condition. The literature shows (7) that some people who struggle with autoimmune problems may be negatively affected by chocolate, so if you are a chocoholic, try going without for a while and seeing if it makes a difference.
Dairy
Casein, the main protein found in milk and other dairy products, can be a trigger for runaway inflammation in the body for those who are susceptible. Ghee/clarified butter and plant-based “dairy” products like almond milk may be preferable and safer for some people because these do not contain casein. Some people with autoimmune disorders can also handle fermented dairy, like grass-fed whole yogurt or kefir, so if you love your dairy products, you might try limiting yourself to these first.
Nightshades
Members of this plant group that consists of tomatoes, peppers, potatoes, eggplants, goji berries, and some spices (like cayenne pepper) contain certain alkaloids in their skins which can cause an inflammatory response (8) in the bodies of some susceptible people.
Instant coffee
Beloved by many on a busy work day, instant coffee (but not brewed coffee) may cause an inflammatory-immune response in some individuals with autoimmune disorders. Why is instant coffee worse? Research points to the chemicals used in the manufacturing of instant coffee, so it may not be the coffee itself.
That said, some individuals respond negatively to regular brewed coffee as well. I run food reactivity blood labs on my patients to see what underlying food triggers they may have, but you can also test yourself by phasing out coffee. After the caffeine headache clears, you may find you feel a lot better.
Artificial Sweeteners
Artificial sweeteners like saccharine (Sweet’N Low), sucralose (Splenda), and aspartame (Equal and NutraSweet) are in many diet and zero-calorie drinks and foods, but even though people may believe that reducing calories with these products is good for health, the fact is that simply eliminating artificial sweeteners and diet soda alone may reverse Hashimoto’s. The mechanism seems to be their proven negative effect on the microbiome.
Stress
Research has found (9) chronic mental stress to be a trigger for autoimmune diseases, and accordingly, many of my patients noticed the onset of their autoimmune health problems during a rough time in their lives. Stressful life events can be the tipping point for an autoimmune response. Stress management techniques like deep breathing and meditation can help to reverse the stress response.
Toxins
Modern living has its benefits, but it has also created a planet so toxic that nobody can avoid exposure to pollution, food additives, heavy metals, cosmetics, and the toxic chemicals in everyday tasks like cleaning and personal hygiene. Studies have shown that these toxins play a role in autoimmune cases such as autoimmune thyroiditis. Avoiding toxic exposure as much as you can gives your body a better chance to detox.
A comprehensive health history and diagnostic testing from a functional medicine practitioner can demonstrate the characteristics of your individual toxic load so you can start detoxing more efficiently and with more targeted detox therapies, allowing your body to focus its energy on immune regulation rather than constant detoxification.
SIBO
Small intestinal bacterial overgrowth, or SIBO, occurs when normal bacteria of the microbiome expand beyond the large intestine into the small intestine, where they are not supposed to be. This can lead to a number of localized autoimmune spectrum conditions, such as IBS and acid reflux. Chronic SIBO can also lead to a leaky gut, which can then trigger more advanced autoimmune problems throughout the body.
Weakened microbiome
Your microbiome – those colonies of bacteria in your gut – controls not only your immune system, but your brain, hormones, and genetic expression. When pathogenic species overgrow, the result can be parasitic, yeast, and fungal infections, which have all been implicated in a variety of autoimmune-spectrum conditions, such as Parkinson’s and Multiple Sclerosis.
You don’t necessarily have to be experiencing gastrointestinal symptoms to be affected by these pathogens. I run a specific two- or three-day stool lab to uncover these often undiagnosed factors in autoimmunity. Getting this kind of test can be informative regarding your microbiome balance.
Leaky gut syndrome
One of the central tenets of functional medicine is that increased gut lining permeability, or a “leaky gut,” is a precursor to autoimmunity. Since all of the above-mentioned triggers can lead to leaky gut syndrome, a leaky gut can be considered a casual trigger, as well as a symptom, of an autoimmune condition. Taking steps to repair the gut can therefore help to avoid triggering flares as well as help to reverse the autoimmune response.
Smoking
By now, everyone knows that smoking is destructive to good health, for genetically susceptible people, it can be especially disastrous. Multiple studies have examined the effects of smoking on people with autoimmune thyroid disorders. One study (10) observed an increase in autoimmune hypothyroidism in women smokers.
Infections
Infections, including bacterial, parasitic, fungal, and yeast, are associated (11) with just about every autoimmune condition. This could be due to the fact that the majority of our immune system is produced from the gut microbiome, so when infections enter the gut, they can alter immune activity.
This can become a trigger for autoimmune thyroid disorders (AITD). In the above study, 36% of Graves’ disease disease patients had evidence of a recent viral or bacterial infection. Avoiding or immediately treating infections may prevent this chain of events.
Iodine
This one may surprise you because iodine is often prescribed as the natural remedy for thyroid problems, but too much iodine can trigger a thyroid storm for those with autoimmunity. It’s true that iodine is required for thyroid hormone production, but several studies have found (12) that increased iodine intake is indeed associated with autoimmune hypothyroidism.
Research has also found (13) an increase in thyroid antibodies with iodine supplementation. This just goes to show that what works for one person may not be right for another, even when it comes to natural treatments.
The 5 Best Supplements For Autoimmune Disease
As Hippocrates, the father of medicine, said “Let food be thy medicine, and medicine thy food.” When there is a lack of nutrients in the foods you’re consuming, the genetic switch for autoimmunity could be triggered, but flooding your body with those nutrients can reverse that trigger.
- Vitamin A
Vitamin A is essential for a strong immune system, and vitamin A deficiency has been linked (14) to autoimmune diseases such as rheumatoid arthritis and type 1 diabetes. (15) Researchers suspect (16) the reason has to do with our dendritic cells, which send out a “red alert” at the sign of a supposed invader, to stimulate immunity. This “calm down” message can be strongly supported by vitamin A, making it possibly the best natural supplement for autoimmune disease.
Food Medicine: True vitamin A, called retinol, is only found in animal products like fish, shellfish, fermented cod liver oil, liver, and butterfat from grass-fed cows. Plant carotenes, a precursor to vitamin A, are found in sweet potatoes and carrots but the conversion rate to the usable retinol is very weak. In fact, research suggests (17) that in healthy adults, just 3% of beta-carotene gets converted in a healthy adult.
- Vitamin D
Known as the “sunshine vitamin,” this nutrient is essential for many metabolic and immunological pathways in the body, but specifically, vitamin D works in conjunction with vitamin A and has been shown to dampen the inflammatory response. With autoimmune conditions like inflammatory bowel disease, multiple sclerosis, psoriasis, and rheumatoid arthritis, Th17 cells run out of control, but Vitamin D can help quell that inappropriate response.
Food Medicine: As with vitamin A, vitamin D is most abundant in animal and dairy fats, but the best way to get it is by soaking up some time in the sun – about 20 to 60 minutes a day, depending on your complexion. Consider getting tested every few months to ensure your vitamin D levels are within a healthy range.
- Vitamin K2
One study (18) in the Journal of Neuroimmunology suggests that vitamin K2 may effectively inhibit inflammation in the brain and spinal cord. Unfortunately, K2 is one of the most common nutrient deficiencies in a modern western diet.
Food Medicine: Vitamin K2 is best paired with other fat-soluble vitamins, A and D, in whole food form like grass-fed butter oil (ghee) or organ meat. Natto, a Japanese superfood made from non-GMO fermented soybeans, also has high levels of K2.
- Iron
Iron deficiency anemia (IDA) is linked to many autoimmune diseases, but it isn’t clear how much of this is cause and how much is effect. One likely reason is that ferritin (stored iron) is mostly absorbed in the intestines. When absorption is compromised by inflammation and autoimmunity, iron stores can fall too low, and as you may already know, damage to the gut lining and leaky gut syndrome are considered (in functional medicine) to be preconditions for autoimmunity.
Food Medicine: Once the gut is healed, iron-rich foods like grass-fed beef, liver, and spinach can be effective, as well as cooking with cast iron cookware.
- Micronutrients
Micronutrient deficiencies – especially of selenium, (19) magnesium, (20) and zinc (21) – are associated with several autoimmune diseases. That’s likely primarily due to chronic inflammation, which decreases the absorption of these vital nutrients. Yet, these micronutrients are required for the healthy production and conversion of the thyroid hormone, and thyroid problems such as Hashimoto’s disease are some of the most common autoimmune conditions.
Food Medicine: A variety of nuts and seeds like Brazil nuts, as well as oysters, are good sources of these nutrients.
10 Tools to Prevent and Reverse Autoimmune Inflammation
While it’s true that, at least when it comes to autoimmune conditions, once that genetic switch has been turned on, it doesn’t turn off again, there is still much you can do to dampen and reverse your autoimmune response. Better yet, this can be done in a way that dramatically reduces or even eliminates symptoms, all without prescription drugs or bouncing around from specialist to specialist with no clear answers. Here's how to prevent autoimmune disease and even reverse your symptoms.
- Have your gut permeability tested
Most of your immune system resides in your gut, but when its protective lining is compromised, an autoimmune response can be the result. To determine the integrity of the gut lining, I run labs so my patients and I can address this major underlying component to regaining health.
- Restore the integrity of your gut lining
Once you know the level of your gut permeability and whether you have any secondary issues like small intestinal bacterial overgrowth (SIBO) or chronic bacterial, yeast, or parasitic infections, you can heal your particular issue. Here is some great general information on natural ways to heal the gut.
- Get your antibodies tested
Depending on your specific autoimmune conditions, you will likely have elevated antibodies, which are proteins that are a part of your immune defense system. Knowing your specific antibody levels will help you do two things: 1) Gauge your healing progress in a measurable way, and 2) Get clues to any associated autoimmune disorders you may have, as many people with autoimmunity have more than one area where this manifests.
- Nix the gluten
Not everyone (arguably) has a negative reaction to gluten, but if you have an autoimmune condition, you don’t need a lab test to tell you that gluten should be on your no list. This protein, which is found in wheat, spelt, rye, and barley, tends to be especially inflammatory and immune-provoking (22) for those with many autoimmune conditions. Though I do run comprehensive gluten intolerance labs for some autoimmune cases to demonstrate definitively the level of intolerance, and to give my patients objective motivation for removing gluten, I can tell you from vast experience that gluten should be off the list for anyone with this health issue. If you aren’t yet convinced, just try eliminating it completely for 60 days, then reintroducing it. This can be a helpful test to demonstrate to people how strongly symptoms return when gluten is reintroduced.
- In addition to gluten, determine your cross-reactive foods and remove them
Sometimes, bodies with overactive immune systems can attack something just because it resembles something else. This is called molecular mimicry, (23) and it can happen when the proteins in a food look like gluten. Even gluten-free grains like corn and rice can flare up the immune system in some people – something I see frequently in my practice. Find out if you are having any cross-reaction with the food you are eating by removing them for 60 days and reintroducing them one at a time to determine if your symptoms return or flare. This can be very helpful for people who have cleaned up their diet but are still having symptoms.
- Detox on the reg
People with autoimmune conditions tend to have altered detoxification pathways, so giving them a helping hand on a daily basis can help get the body back into shape. The best way to do this is to eat a variety of green leafy vegetables like kale and spinach and avoid sugar and processed foods that make the toxic load heavier. These two things alone can make a big difference in your health.
- Add powerful food medicines into your diet
Foods such as green tea and turmeric have been shown (24) to dampen the autoimmune response in the body, especially in the brain. Have a cup of green tea and add turmeric to your food daily for a huge anti-inflammatory and immune-balancing boost.
- Replace refined table salt with natural sea salt
Table salt is highly processed and has been shown (25) to aggravate and increase some autoimmune conditions. Go with more natural salt that contains trace minerals.
- De-stress daily
When it comes to the “fire” of autoimmunity, stress is the gasoline. In fact, stressful events are often the triggers for autoimmunity. Many of my patients say they noticed the onset of their condition during a particularly stressful life event. Don’t let stress aggravate your health a minute longer. Regular practice of meditation, yoga, tai chi, or other stress-relieving practices can help you better manage stress and balance your immune system.
- Go for glutathione
Many people in poor health are deficient in this important nutrient, (26) so eat plenty of sulfur-rich vegetables like onions, cabbage, and broccoli to aid in methylation, a biochemical pathway that produces glutathione naturally.
Your Efforts Will Be Worth It
Autoimmune disease is not curable but can be manageable with natural interventions that might even put your autoimmune disease into remission. Consistently practicing these ten steps is a great way to begin reversing autoimmune disease symptoms and living a vibrant, healthy life. I’ve seen countless people with life-destroying autoimmune symptoms completely regain their health through natural lifestyle changes like these. Will you be next?
As one of the first functional medicine telehealth clinics in the world, we provide webcam health consultations for people around the globe.
Photo: Stocksy
Read Next: Dysautonomia: Types, Symptoms, Root Causes, And Treatment Options
Start Your Health Journey Today
FUNCTIONAL MEDICINE CONSULTATIONS FOR PEOPLE AROUND THE WORLD
References:
- Marrack, P., Kappler, J. & Kotzin, B. Autoimmune disease: why and where it occurs. Nat Med 7, 899–905 (2001). https://doi.org/10.1038/90935
- Fasano A. Zonulin, regulation of tight junctions, and autoimmune diseases. Ann N Y Acad Sci. 2012;1258(1):25‐33. doi:10.1111/j.1749-6632.2012.06538.x
- Brodin P, Jojic V, Gao T, et al. Variation in the human immune system is largely driven by non-heritable influences. Cell. 2015;160(1-2):37‐47. doi:10.1016/j.cell.2014.12.020
- Steinman, L. A brief history of TH17, the first major revision in the TH1/TH2 hypothesis of T cell–mediated tissue damage. Nat Med 13, 139–145 (2007). https://doi.org/10.1038/nm1551
- Adrenal Insufficiency & Addison’s Disease NIH https://www.niddk.nih.gov/health-information/endocrine-diseases/adrenal-insufficiency-addisons-disease
- Rose NR. Predictors of autoimmune disease: autoantibodies and beyond [published correction appears in Autoimmunity. 2008 Dec;41(8):691]. Autoimmunity. 2008;41(6):419‐428. doi:10.1080/08916930802031686
- A. Vojdani and I. Tarash, "Cross-Reaction between Gliadin and Different Food and Tissue Antigens," Food and Nutrition Sciences, Vol. 4 No. 1, 2013, pp. 20-32. doi: 10.4236/fns.2013.41005.
- Patel B, Schutte R, Sporns P, Doyle J, Jewel L, Fedorak RN. Potato glycoalkaloids adversely affect intestinal permeability and aggravate inflammatory bowel disease. Inflamm Bowel Dis. 2002;8(5):340‐346. doi:10.1097/00054725-200209000-00005
- Ljudmila Stojanovich, Dragomir Marisavljevich Stress as a trigger of autoimmune disease Autoimmunity Reviews Volume 7, Issue 3, January 2008, Pages 209-213. doi:10.1016/j.autrev.2007.11.007
- Vestergaard P, Rejnmark L, Weeke J, et al. Smoking as a risk factor for Graves' disease, toxic nodular goiter, and autoimmune hypothyroidism. Thyroid. 2002;12(1):69‐75. doi:10.1089/105072502753451995
- Tomer Y, Huber A. The etiology of autoimmune thyroid disease: a story of genes and environment. J Autoimmun. 2009;32(3-4):231‐239. doi:10.1016/j.jaut.2009.02.007
- Sun X, Shan Z, Teng W. Effects of increased iodine intake on thyroid disorders. Endocrinol Metab (Seoul). 2014;29(3):240‐247. doi:10.3803/EnM.2014.29.3.240
- Boukis MA, Koutras DA, Souvatzoglou A, Evangelopoulou A, Vrontakis M, Moulopoulos SD. Thyroid hormone and immunological studies in endemic goiter. J Clin Endocrinol Metab. 1983;57(4):859‐862. doi:10.1210/jcem-57-4-859
- Ikeda U, Wakita D, Ohkuri T, et al. 1α,25-Dihydroxyvitamin D3 and all-trans retinoic acid synergistically inhibit the differentiation and expansion of Th17 cells. Immunol Lett. 2010;134(1):7‐16. doi:10.1016/j.imlet.2010.07.002
- Susan J. Zunino, David H. Storms, Charles B. Stephensen, Diets Rich in Polyphenols and Vitamin A Inhibit the Development of Type I Autoimmune Diabetes in Nonobese Diabetic Mice, The Journal of Nutrition, Volume 137, Issue 5, May 2007, Pages 1216–1221, https://doi.org/10.1093/jn/137.5.1216
- Manicassamy S, Ravindran R, Deng J, et al. Toll-like receptor 2-dependent induction of vitamin A-metabolizing enzymes in dendritic cells promotes T regulatory responses and inhibits autoimmunity. Nat Med. 2009;15(4):401‐409. doi:10.1038/nm.1925
- Hedrén E, Diaz V, Svanberg U. Estimation of carotenoid accessibility from carrots determined by an in vitro digestion method. Eur J Clin Nutr. 2002;56(5):425‐430. doi:10.1038/sj.ejcn.1601329
- Moriya M, Nakatsuji Y, Okuno T, Hamasaki T, Sawada M, Sakoda S. Vitamin K2 ameliorates experimental autoimmune encephalomyelitis in Lewis rats. J Neuroimmunol. 2005;170(1-2):11‐20. doi:10.1016/j.jneuroim.2005.08.001
- Negro R. Selenium and thyroid autoimmunity. Biologics. 2008;2(2):265‐273. doi:10.2147/btt.s2746
- Mooren FC, Golf SW, Völker K. Effect of magnesium on granulocyte function and on the exercise induced inflammatory response. Magnes Res. 2003;16(1):49‐58.
- Chika Kitabayashi, Toshiyuki Fukada, Minoru Kanamoto, Wakana Ohashi, Shintaro Hojyo, Toru Atsumi, Naoko Ueda, Ichiro Azuma, Hiroshi Hirota, Masaaki Murakami, Toshio Hirano, Zinc suppresses Th17 development via inhibition of STAT3 activation, International Immunology, Volume 22, Issue 5, May 2010, Pages 375–386, https://doi.org/10.1093/intimm/dxq017
- Zonulin and Its Regulation of Intestinal Barrier Function: The Biological Door to Inflammation, Autoimmunity, and Cancer Alessio Fasano Physiological Reviews 2011 91:1, 151-175
- Cusick MF, Libbey JE, Fujinami RS. Molecular mimicry as a mechanism of autoimmune disease. Clin Rev Allergy Immunol. 2012;42(1):102‐111. doi:10.1007/s12016-011-8294-7
- Wu D, Wang J, Pae M, Meydani SN. Green tea EGCG, T cells, and T cell-mediated autoimmune diseases. Mol Aspects Med. 2012;33(1):107‐118. doi:10.1016/j.mam.2011.10.001
- Katherine Harmon Salt Linked To Autoimmune Diseases Nature 06 March 2013. https://www.nature.com/news/salt-linked-to-autoimmune-diseases-1.12555
- Richie JP Jr, Nichenametla S, Neidig W, et al. Randomized controlled trial of oral glutathione supplementation on body stores of glutathione. Eur J Nutr. 2015;54(2):251‐263. doi:10.1007/s00394-014-0706-z
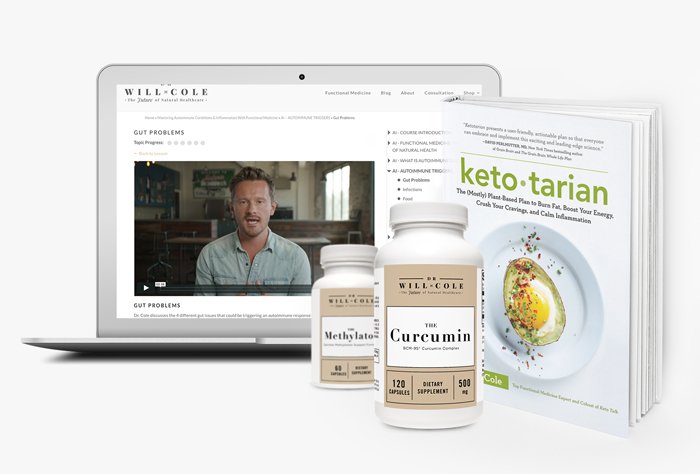
View More At Our Store
Purchase personally curated supplements
and Dr. Will Cole’s books!
The information on this website has not been evaluated by the Food & Drug Administration or any other medical body. We do not aim to diagnose, treat, cure or prevent any illness or disease. Information is shared for educational purposes only. You must consult your doctor before acting on any content on this website, especially if you are pregnant, nursing, taking medication, or have a medical condition.
Our articles may include products that have been independently chosen and recommended by Dr. Will Cole and our editors. If you purchase something mentioned in this article, we may earn a small commission.

BY DR. WILL COLE
Dr. Will Cole, DNM, IFMCP, DC is a leading functional medicine expert who consults people around the globe, starting one of the first functional medicine telehealth centers in the world. Named one of the top 50 functional and integrative doctors in the nation, Dr. Will Cole provides a functional medicine approach for thyroid issues, autoimmune conditions, hormonal imbalances, digestive disorders, and brain problems. He is also the host of the popular The Art of Being Well podcast and the New York Times bestselling author of Intuitive Fasting, Ketotarian, Gut Feelings, and The Inflammation Spectrum.

Gut Feelings
Healing The Shame-Fueled Relationship
Between What You Eat And How You Feel
