Your Functional Medicine Guide To Underlying Thyroid Dysfunctions + How To Heal

The thyroid is something that is often the source of many health problems. Low thyroid function, or hypothyroidism, affects around 20 million Americans, and 1 in 8 women will experience a thyroid issue in her lifetime.
The most common cause of low thyroid function is the autoimmune condition, Hashimoto’s disease. If you are faced with this condition there are a few underlying factors to consider when looking to treat your symptoms.
Hashimoto’s disease or autoimmune thyroiditis and was the first autoimmune disease to be discovered in 1912. Your immune system works to keep you healthy by fighting off viruses and bacteria that threaten your body. However, autoimmune conditions occur when your immune system mistakes parts of your body as a threat and ends up attacking itself. This is considered an autoimmune response.
To diagnose Hashimoto’s, you’ll run thyroglobulin antibodies (TGB Ab) and thyroid peroxidase antibodies (TPO Ab) tests. Normally, doctors don’t run these tests because thyroid hormone replacement drugs would be the treatment regardless if you have true primary hypothyroidism or Hashimoto’s. Since the autoimmune response has both active and dormant states, it is vital to look at your entire health history in the case of a false negative test.
Out of all the hypothyroid cases in America, 90 percent are autoimmune. (1) In fact, thyroid related autoimmune conditions affect an estimated 8 percent of the population. In conventional medicine it doesn’t matter if you have a dysfunction with thyroid hormone conversion, primary hypothyroidism, or an autoimmune disease, they will look at treatment the same. However, when it comes to Hashimoto’s the thyroid isn’t actually the problem, making thyroid hormone replacement medication unhelpful. The thyroid is merely the victim of the immune system’s attacks.
Unfortunately, hypothyroidism is so common that it can often be disregarded. “Here’s your prescription. And there’s the door.” The reality, though, is that if your thyroid isn’t working well, nothing in your body will. This master gland that is located in your neck controls many, far-reaching facets of your health, and every cell in your body contains a thyroid hormone receptor.
Article continues below
13 Signs of Thyroid Dysfunction - Thyroid Health
1. Your bones are weak
If you have weak bones, have your thyroid checked. Abnormal thyroid function can decrease (2) bone mineral density. Serum calcium will typically be in the “normal” reference range with hypothyroidism, but outside of the functional, optional range. Over time, this decreasing bone density can lead to fractures.
2. You have gut problems
Among many of the other processes controlled by thyroid hormones is digestion, and low thyroid function can reduce the movement (3) of your intestines, which is of course an essential part of healthy digestion. Poor thyroid function also compromises your body’s ability to absorb nutrients. Healthy thyroid function dampens gut inflammation, so low thyroid function can furthermore be linked with gastric ulcers and leaky gut syndrome.
3. You are experiencing a low sex drive
Although many people think a reduced sex drive is just due to aging, in fact it may be a symptom of abnormal hormone function. Thyroid hormones affect the metabolism of estrogen and testosterone in the body and thyroid hormone problems can cause low libido in both men and women. Also, hypothyroidism in men is linked (4) with erectile dysfunction.
4. You are having trouble with your weight
When your thyroid hormones are low, your body will be less able to break down fat, which can quickly add pounds or make you resistant to weight loss despite your efforts at dieting or working out. These efforts don’t address the underlying problem because weight gain isn’t the cause of your problems, but a symptom of something else that is not being addressed. Weight loss happens when you get healthy to lose weight, not the other way around. When you restore thyroid function, weight loss will be the natural byproduct.
5. Your energy is lacking
In addition to slowing your ability to burn fat, hypothyroidism will also decrease your energy, causing debilitating fatigue.
6. You develop blood sugar problems
When your body is in a low thyroid state, it decreases your body’s ability to absorb glucose or blood sugar. Glucose needs to get into your cells in order to create ATP, your cellular energy source. Despite sluggish glucose metabolism, many people struggling with low thyroid hormones can feel hypoglycemic, (5) like they have low blood sugar. Because the cells are not getting the glucose they need, you can feel like you are hypoglycemic even with normal looking blood sugar labs. This vicious cycle of hormonal dysfunction can lead to metabolic syndrome or insulin resistance.
7. You tested positive for high cholesterol and triglycerides
Sluggish thyroid hormone levels decrease the breakdown (6) of cholesterol, which can lead to elevated total cholesterol and triglycerides. While high cholesterol alone is a poor predictor for heart attack and stroke risk, elevated triglycerides is an accurate marker for these life-threatening health emergencies.
8. You suspect you have adrenal fatigue
When you have hypothyroidism, it puts stress on your hypothalamic-pituitary-adrenal (HPA) axis. Because of the lack of glucose and energy getting to the cells, the brain signals the adrenals to produce more cortisol in an attempt to get more energy into the cells. This further complicates your hormonal health picture and can lead to HPA axis dysfunction and eventually, adrenal fatigue.
9. You are overloaded with toxins
Your liver and your gallbladder do the heavy lifting when it come to the removal of toxins you ingest or that are the by-products of metabolism. Poor thyroid health can inhibit optimal function of your liver and gallbladder, which can significantly decrease your body’s ability to rid itself of toxins. This may also cause nonalcoholic fatty liver disease. (7) Impaired detoxification pathways are common in patients dealing with thyroid problems.
10. You have estrogen dominance or deficiency
Estrogen comes in the form of three metabolites: Estrone (E1), estradiol (E2), and estriol (E3). You need just the right amount of each of these for optimal health, but when your thyroid isn’t working well, it can unbalance your estrogen metabolite ratio.
11. You experience brain problems
Poor neurotransmitter expression and an increased risk of mental health problems such as depression, anxiety, and bipolar disorder can be linked to hypothyroidism, due to the fact (8) that the brain contains a predominance of thyroid receptor sites. Also, people with depression had higher rates of thyroid conversion impairments, or low T3 syndrome, according to one 2014 study. (9)
12. You get hot flashes or cold spells
When your thyroid hormone levels are low, it affects your body’s temperature control. This can cause you to feel cold all the time, or have night sweats and hot flashes.
13. You are losing hair
Since thyroid hormones are one determining factor of metabolic rate and nutrient absorption, thyroid dysfunction can lead to hair loss. (10) Regaining hair health means optimizing thyroid hormone levels.
Underlying Causes For Thyroid Dysfunction
In order to successfully treat hypothyroidism, we need to understand what triggers the immune system to attack the thyroid in the first place. Only then can we begin to mitigate these triggers to start a path to true healing.
1. Stress
Research has confirmed the stress-thyroid connection. Two studies, one from 1991 (11) and the other from 2001, (12) both found that autoimmune thyroid patients had more stressful life events before their diagnosis, compared to control groups.
This could be due to the effect stress has on your thyroid hormone function. Your main stress hormone, cortisol, can block conversion of T4 to the active T3, and can also increase the unusable reverse T3 (rT3), further confusing the delicate balance of thyroid hormones that are so essential for good health. Many of my patients discover that their thyroid problems started after a stressful time in their lives.
Be consistent with stress-busting practices like mindfulness meditation and yoga. These activate your body’s parasympathetic nervous system, which will make you feel more zen, while also boosting healthy thyroid function.
2. Food intolerances
If you are predisposed to an autoimmune condition, certain foods can cause your immune system to overreact. Specific foods such as grains, gluten, soy, and dairy can contribute (13) to inflammation which can further perpetuate symptoms and autoimmune flare-ups.
You don’t have to have celiac disease to have a gluten intolerance – the inflammatory effects of gluten were shown (14) to last up to six months each time you eat it, even in those without celiac disease.
Imagine what happens when you eat it every day! You can see the far-reaching effects of this protein and its resultant long-term inflammatory response. Conventional medicine practitioners typically don’t run the proper tests to see if this is a trigger in individual cases, but in functional medicine, we often see this connection.
I run a full food intolerance panel to help you determine which foods are an issue for you.
3. Nutrient deficiencies
Your body relies on a certain amount of specific nutrients for your immune system to function optimally. Deficiencies in selenium (15) and vitamin D (16) have been linked to poor immune function in people with autoimmune thyroid conditions.
4. Gut problems
Close to 80 percent of your immune system is found in your microbiome. A compromised gut like in leaky gut syndrome or bacterial imbalances will contribute (17) to poor immune health. Also, 20 percent of your T4 is converted to T3 in the gut, and an imbalanced, unhealthy microbiome can inhibit this process. Gut labs can determine your level of gut dysfunction to see if this is a factor in your health case.
5. Toxin exposure
Our world has become increasingly toxic. Studies have shown that chemicals and heavy metals can cause an autoimmune response (18) against the thyroid. You can measure your toxicity levels through labs such as a urine heavy metal panel.
6. Estrogen imbalances
Proper levels of hormones are important for optimal health. An imbalance of estrogen in women has been shown to trigger autoimmune thyroid problems.
7. Blood sugar dysregulation
PCOS, insulin resistance, or other blood sugar problems can contribute and perpetuate Hashimoto’s.
8. Iodine levels
While iodine is necessary to make thyroid hormones, excess amounts can actually exacerbate Hashimoto’s symptoms. (19) Research has also found (20) an increase in thyroid antibodies with iodine supplementation. Since iodine is an active ingredient in many thyroid supplements, it just goes to show that what works for one person, doesn’t always work for the next.
9. Infections
Infections, including bacterial, parasitic, fungal, and yeast, are associated (21) with just about every autoimmune condition. This could be due to the fact that the majority of our immune system is produced from the gut microbiome, so when infections enter the gut, they can alter immune activity.
This can become a trigger for autoimmune thyroid disorders (AITD). In the above study, 36% of Graves’ disease disease patients had evidence of a recent viral or bacterial infection. Avoiding or immediately treating infections may prevent this chain of events.
Read Next: How To Overcome Graves Disease Through Diet
10. Artificial Sweeteners
Artificial sweeteners like saccharine (Sweet’N Low), sucralose (Splenda), and aspartame (Equal and NutraSweet) are in many diet and zero-calorie drinks and foods, but even though people may believe that reducing calories with these products is good for health, the fact is that simply eliminating artificial sweeteners and diet soda alone may reverse Hashimoto’s. The mechanism seems to be their proven negative effect on the microbiome.
11. Smoking
By now, everyone knows that smoking is destructive to good health, for genetically susceptible people, it can be especially disastrous. Multiple studies have examined the effects of smoking on people with autoimmune thyroid disorders. One study (22) observed an increase in autoimmune hypothyroidism in women smokers, while another study showed an increase in Graves’ disease in smokers.
But studies have shown that a decrease (23) in thyroid function could be reversed by taking n-acetylcysteine (NAC), and by increasing the super-antioxidant glutathione.
12. Low vitamin A
Low vitamin A can spell trouble for your thyroid because this fat-soluble vitamin has been shown (24) to boost T3 levels and normalize TSH.
True vitamin A, called retinol, is only found in animal products like fish, shellfish, fermented cod liver oil, liver, and butterfat from grass-fed cows. Plant carotenes, a precursor to vitamin A, are found in sweet potatoes and carrots, but the conversion rate to the usable retinol is very weak. In fact, research suggests (25) that just 3 percent of beta-carotene gets converted in a healthy adult. So eat up those animal fats!
13. Low selenium
Selenium is essential (26) to convert T4 to T3 in your liver. Selenium also protects (27) against autoimmune thyroid problems.
Eat a variety of nuts and seeds, especially Brazil nuts, as well as oysters, another good source of selenium.
14. Low iron
Iron is needed (28) for the production of thyroid peroxidase, the enzyme used to make your thyroid hormones.
If you have low iron, the most important thing to discover first is the underlying problem that’s causing the iron deficiency. Healing your gut is essential for healthy nutrient absorption, especially iron. Once the gut is healed, iron-rich foods like grass-fed beef, liver, and spinach can be effective – as can cooking with cast-iron cookware.
15. Low copper
Healthy copper levels were found (29) to increase total T4 and T3 levels.
The best way to get bioavailable copper is by eating grass-fed liver and oysters. Sesame seeds are a good plant source as well.
16. Hormone imbalances
Your hormones are all connected, and the ripple effect from dysfunction in one endocrine gland outputting any hormone can negatively affect your thyroid. Low estrogen, (30) insulin resistance, and low testosterone (31) were all found to inhibit thyroid function. Depending on your individual hormone problems, solutions will vary.
17. Pain
Being in chronic pain has been shown (31) to suppress deiodinase, the liver enzyme that converts 80 percent of your T4 into your active T3.
There is no simple answer for this. No one chooses to be in chronic pain, but there are many therapies that may help. I have seen some success with liposomal turmeric, which has great bioavailability compared to the standard version of this anti-inflammatory natural product.
The 6 Different Types of Underlying Thyroid Problems
While some are more common than others, there are actually a few different thyroid problems you could be experiencing due to the fact that thyroid physiology is complex and unique to the individual.
So when you have thyroid-related symptoms such as fatigue or weight gain, your problem may be more complex than something that can be fixed with a simple thyroid hormone replacement drug. (And no, thyroid dysfunction is not a sign of “just getting older,” as you may have been told.) You may even have thyroid symptoms despite “normal” labs.
Unfortunately, there’s no such thing as a magic thyroid-fixing pill for everyone. Instead of diagnosing “low thyroid,” functional medicine doctors prefer to make a more comprehensive diagnosis, to gain insight into why someone is struggling with the symptoms they have.
Here are six hidden thyroid problems we need to start talking about and what to do about each one:
1. Autoimmune thyroid problems
Research estimates (32) that up to 90 percent of all cases of hypothyroidism are autoimmune in nature, with the most common manifestation being Hashimoto’s disease. When this happens, your thyroid is not the source of the problem, but the victim of a misguided immune system attack, in which your body mistakes your thyroid for a virus.
In mainstream medicine, you typically receive the same thyroid medication whether you have true primary hypothyroidism or an autoimmune disease attacking your thyroid, but in functional medicine we tend to treat autoimmune thyroid problems more naturally and can be different for each individual – since every person has their own unique biochemistry.
Labs to run: Thyroid peroxidase and TBG antibodies
What to do: There’s a lot you can do to naturally manage this condition. I recommend healing the gut with tools such as the elimination diet as well as taking in natural compounds such as Baicalin (33) to promote regulatory T cell (Treg), to balance the immune system.
2. Thyroid resistance
This thyroid dysfunction is also not a primary thyroid problem but a cell receptor issue. Every cell of your body depends on thyroid hormones to function the way they should, but if your cells receptor sites are blunted because of inflammation or toxins, your body will feel the effects of hypothyroidism despite having adequate hormone production, since those hormones aren’t getting where they need to go. In this case, your TSH test will be “normal” but you’ll feel miserable.
Labs to run: Markers such as CRP and homocysteine as well as reverse T3 can shed light on inflammation levels as well as hormone receptor site availability. High triglycerides and low HDL can be signs of insulin resistance, which is another clue because it typically occurs with thyroid resistance.
What to do: Liposomal turmeric and resveratrol are two of my favorite supplements for quelling excessive inflammation.
3. Elevated thyroid-binding globulin
This is a common scenario when a woman has high estrogen levels. I also see it in women using birth control pills or estrogen creams. All hormones get transported throughout the body on protein carriers. The thyroid’s specific transport carriers are called thyroid-binding globulins (TBG.) When TBG levels are elevated, this could cause an increase of protein-bound thyroid hormones, which can’t be used by your body.
Labs to run: TBG, Free T3, and T4 as well as an expanded female hormone panel.
What to do: Clear excess hormones by supporting detoxification pathways with herbs such as milk thistle, and by supporting methylation pathways with activated B vitamins.
4. Hypothyroidism second to pituitary hypofunction
Your thyroid only does what your brain tells it to do, and if your pituitary gland isn’t working well (this could be due to chronic stress, chronic infections, or even a benign pituitary tumor), the hypothalamic-pituitary-thyroid (HPT) axis will malfunction. This is the communication line between your brain and thyroid. When the pituitary gland, which sits at the base of your brain, isn’t communicating with your thyroid gland, then the thyroid may be just fine. It’s just that nobody is giving the signal that it’s time to get to work!
Labs to run: Look for low levels of T4 and T3 despite a normal-to-low TSH, and possibly viral labs, such as the one that checks for the Epstein-Barr virus (EBV.)
What to do: To support pituitary health and optimal HPA communication, I recommend natural brain-immune support tools, such as astragalus, olive leaf, rubidium, sage leaf, L-lysine, zinc, and vitamin C.
5. Thyroid under-conversion
This pattern, also called low T3 syndrome, is common with chronic adrenal stress and its related elevated cortisol. The majority of thyroid hormone comes in the form of T4, which is largely metabolically inactive and has to be converted to T3 for use in the body. It’s estimated that 80 percent of thyroid conversion happens in your liver and 20 percent in your gut.
Through this process, a special enzyme called 5′ deiodinase takes one iodine molecule off of T4 to make it the active T3. This pattern has been covered in medical literature for years but is not effectively alleviated by the thyroid replacement hormones. Most thyroid drugs are synthetic T4, which isn’t the problem in this pattern.
Labs to run: Free and total T3, liver enzymes, microbiome testing, and nutrient testing of selenium, magnesium, and zinc.
What to do: In addition to getting your adrenal fatigue, gut, and liver health under control, foods rich in selenium, zinc, and magnesium help make the enzyme needed for healthy thyroid conversion. Brazil nuts and shellfish, such as oysters, are some of my favorite options.
6. Thyroid over-conversion
This thyroid pattern is sometimes found in people with elevated testosterone levels, insulin resistance, type 2 diabetes, and in women with PCOS (polycystic ovarian syndrome.) You would think that if the body produces more T3, the metabolically active form of thyroid hormone, it would be a good thing. However, as with just about everything, too much of a good thing isn’t such a good thing. Over-conversion of T3 can overwhelm your cell receptors, leading them to become resistant to the T3, so even though you have a lot, once again, you aren’t able to use it.
Labs to run: Free and total T4 and T3, free and serum testosterone, fasting blood sugar, and HbgA1c.
What to do: In addition to eating a clean diet consisting of lots of vegetables, fruits, meats, and healthy fats, I recommend natural medicines such as alpha-lipoic acid and chromium supplements, along with cinnamon, all of which can act as blood sugar balancers.
As for general thyroid health, sea vegetables such as dulse, nori, and arame are great nutrient sources, including the vitally important iodine. You need iodine from foods to fuel thyroid hormone production.
A Functional Medicine Guide To Thyroid Labs
Diagnosing a thyroid issue isn't easy because lab test results can be confusing and misleading. If your doctor only tests for your level of thyroid-stimulating hormone, or TSH, then you will only get treated (with a synthetic thyroid hormone like Synthroid or levothyroxine) if your labs are out of range. If your labs come back "normal," you will probably be sent home with a shrug or an assurance that you are fine. In my view, this is a serious problem.
How Labs Determine “Normal” Ranges
If you have the symptoms of low thyroid hormone but your TSH is “normal,” something is not being addressed. Part of the problem starts with the reference range for what is considered normal. How do we get the “normal” lab range? The reference range is based on a statistical average of the population getting tests out of the lab. This is why (other than for vitamin D and cholesterol levels) lab reference ranges will vary depending on the lab.
The people who get tested in labs – in other words, the population of that lab – are obviously statistically not the healthiest segment of the population. Otherwise, they wouldn’t be getting lab tests. That means if the lab results are “normal” despite your symptoms, what your doctor is essentially saying is you’re just like a lot of other sick people!
In functional medicine, we look at a much narrower range of normal, taking this into account. We want your labs to look like a bunch of healthy people whose bodies function optimally and who feel great.
Thyroid Labs: The Functional Medicine Version
A functional medicine look at your thyroid is more in depth than just a TSH and maybe a T4. We do a broader range of tests and look at a narrower range of optimal results. Here are some of the labs I run on my patients, what they actually mean, and what kind of results are ideal:
TSH
Thyroid-stimulating hormone is released from your pituitary gland to communicate with your thyroid. If your TSH is high, it’s sort of like your brain shouting at your thyroid to work harder. Research has linked (34) a lab “normal” TSH of 2.5-3.5 mlU/mL with a 69% risk of dying from a heart attack or stroke. Now you can see why the optimal (functional) range is so important for your health. Forget the larger reference ranges and aim for what’s optimal:
Lab range: .45-5.5 mlU/L
Optimal range: 0.5-2.0 mlU/L
Total T4
T4 is mostly metabolically inactive in the body and has to be converted to T3 to be usable. This lab gives you a total of unbound and bound forms of T4. Hormones have to be unbound from the protein carrier to be used by your body. Because of this, this lab doesn’t give us the activity of T4 when measured alone. T4 is measured in conjunction with a T3 uptake.
Lab range: 4.5-12 mcg/DL
Optimal range: 6.0-12.0 mcg/DL
T3 Uptake
This lab doesn’t look directly at T3, but is very useful at indirectly looking at other hormones such as estrogen or testosterone and their relation with the binding of thyroid hormones.
Lab range: 22-35%
Optimal range: 25-38%
Total T3
This lab shows us the total amount of the metabolically active thyroid hormone. It allows a doctor to check your body’s ability to convert T4 to T3 and to rule out an overactive thyroid.
Lab range: 80-200 ng/DL
Optimal range: 100-180 ng/DL
Free T4
This will tell you the levels of free or active form of T4. This will be low in cases of hypothyroidism but can be normal in subclinical, early stages of thyroid dysfunction.
Lab range: 0.8-1.8 ng/DL
Optimal range: 1.0-1.5 ng/DL
Free T3
This is the more active, usable form of your thyroid hormone. Low T3 syndromes are a common dysfunction that I see in practice, and a low level of this hormone is strongly linked (35) to a higher risk of heart attack. The problem, if you’re taking a synthetic T4 medication, is that your body isn’t converting the hormone properly into T3, though there are many reasons your thyroid medication may not be working.
Lab range: 2.3-4.2 pg/mL
Optimal range: 3.0-4.0 pg/mL
Reverse T3
Chronic stress and high cortisol can raise levels of reverse T3, which is an unusable form of the thyroid hormone.
Lab range: 8-25 ng/DL
Optimal range: < 15 ng/DL
Thyroid Antibodies
High levels of thyroid antibodies show an autoimmune attack against the thyroid. The overwhelming majority of low thyroid cases are on the autoimmune spectrum, the most common being Hashimoto’s disease.
Thyroid Peroxidase (TPO) Ab optimal range: < 9 IU/mL
Thyroglobulin Ab optimal range: 0-0.9 IU/mL
In addition to these thyroid-focused labs, functional medicine practitioners are likely to recommend additional labs to address your microbiome, immune system, and other hormones. These should also be considered for the most complete picture of what is going on with your health.
Getting the big picture from labwork is a solid first step towards finding out exactly what is going on with your thyroid. What conventional doctors may not tell you is that there are many thyroid dysfunctions that typically don’t show up on labs, and that throwing synthetic thyroid medication at the problem will, in many cases, not do enough to relieve symptoms. You can do more to help.
The Uncomfortable Truth Behind Thyroid Medications
Treatment of thyroid disorders in conventional medicine is, in my opinion, inadequate. Patients with hypothyroidism are typically given a thyroid replacement hormone as medication and care stops there. Because of this, some people still experience low thyroid symptoms despite medication and “normal” labs. The reason is that many thyroid problems are not actually problems of inadequate thyroid hormone. My patients often ask me which thyroid medication is right for them or whether they even need to be on one in the first place. Here is my functional medicine perspective.
What are my options for thyroid medicines?
Thyroid replacement hormones are one of the most commonly prescribed medications. Here is a rundown of the most common prescriptions:
Synthetics
Levothyroxine: This is the most common thyroid hormone. This synthetic T4 hormone comes in over 30 different brand names such as Synthroid and Levothroid.
Liothyronine: This is the generic name for synthetic T3, the active form of the thyroid hormone. The most common brand name is Cytomel.
Natural Sources
- Armour
- Nature-throid
- Westhroid
- compounded thyroid hormones
These naturally sourced supplements come from pig thyroid tissue. Because they are natural, they contain both T4 (the less active hormone that has to be converted in the liver and gut) and T3 (the more biologically active form) hormone.
Many primary care physicians and endocrinologists are only comfortable prescribing the synthetic replacement hormones because decades ago, there was less standardization with natural options. Today, this is not as much of a concern and when thyroid hormone replacement is necessary, I prefer natural options (these are obviously not vegan friendly, if that is a concern for you).
However, these drugs aren’t right for everyone, synthetic or natural, since everyone is different and there is no “one size fits all” or magic pill for thyroid dysfunction. This brings me to the next question I am frequently asked:
I’m on a thyroid medication but it isn’t working for me. Why not?
If you’re still having low thyroid symptoms despite medication, it’s probably not that “you’re just depressed” or “just getting older.” Here are some other factors you should consider:
1. Thyroid drugs contain fillers
Thyroid drugs are pretty comparable as far as their active ingredients, with the biggest variable being the inactive ingredients. Because everyone is different, and many thyroid problems are autoimmune in nature, the fillers used in these pills may be causing a negative response. Drug formulas can change, so it’s important to check your individual medication. If you think you might be having a reaction, immunological labs can uncover certain intolerances you may be having.
Some common inactive ingredients found in thyroid medications that you may react to include:
- dyes
- cellulose
- lactose
- other sugars
- extra iodine (excess iodine can trigger autoimmune thyroid problems)
- corn starch
- modified food starch (may contain gluten, which can trigger autoimmune thyroid problems)
2. “Normal” lab ranges may not be normal
On your lab, you’ll see a “Reference Range.” This range is what’s considered normal in mainstream medicine. That range is based on a bell curve – a statistical average of the population of that particular lab you went to. People who go to labs are typically sick people, so if your result comes back within that reference range, it doesn’t automatically mean it’s at the optimal level for you.
In functional medicine, we look at a narrower and more personalized range of “normal,” so you may find that while a conventional doctor says you are “normal,” a functional medicine doctor will disagree. In addition to tweaking this reference range, your functional medicine doctor may also want to run more expansive thyroid tests to help uncover your exact issues.
3. You might have underlying thyroid dysfunctions
Sometimes there are other thyroid problems that won’t be solved by a pill alone. Thyroid conversion problems and Hashimoto’s disease (autoimmune thyroiditis) are two often overlooked underlying thyroid issues that should be ruled out before defaulting to a pill as the only treatment.
4. You might have inflammation
Inflammation can significantly inhibit thyroid hormone function. Addressing this means dealing with the underlying causes of inflammation, including a poor diet, stress, and toxins. Thyroid hormone resistance, similar to insulin resistance, is one reason why your thyroid medication may not be working for you. I recommend working with a qualified functional medicine practitioner to uncover and address chronic inflammation.
5. You might be experiencing decreased absorption
There are several medications that alter the absorption of activity of T4, a hormone produced by the thyroid. These might include commonly prescribed drugs like antacids, antibiotics, and antifungals, antiarrhythmia medications, cholesterol-lowering medications, diabetic medications, diuretics, hormone replacements, and pain medications.
Some foods may decrease the absorption of thyroid hormones, such as soy-based and high-fiber foods. Iron and calcium supplements can also inhibit thyroid hormone function.
According to the drug manufacturers, it’s best to take your medications four hours before or after you ingest foods, drugs, or supplements that can affect its effectiveness.
6. You might have other health problems
There are other underlying health problems that can both mimic low-thyroid symptoms and also complicate healthy thyroid function. Candida overgrowth, leaky gut syndrome, adrenal fatigue, and other underlying metabolic problems should all be investigated along with thyroid dysfunction, as they are common co-issues.
The Real Reasons Why Your Thyroid Medications Aren't Working
First of all, thyroid medication normally comes in the form of a synthetic T4 thyroid hormone. T4 is the main thyroid hormone that your body produces naturally, but it needs to be converted into T3 for it to be used actively in the body. I have found that the overwhelming majority of people struggling with low thyroid symptoms are having some sort of autoimmune response, in which the immune system mistakes the thyroid as a foreign body and attacks it, destroying it so it cannot produce the thyroid hormones your body needs.
This immune dysregulation can cause systemic inflammation in the body. Inflammation is a normal response to an injury, but when the source of the inflammation, in this case an autoimmune response, isn’t addressed, the vicious cycle of systemic inflammation is never broken. Adding a synthetic hormone to replace what your thyroid isn’t making is only a drop in the bucket in terms of addressing the symptoms that result from this cascade of dysfunction. Not only that, but your body may not be capable of using the hormone you are taking every day.
The only way to actually repair this problem is to address the underlying issues of an autoimmune pattern and inflammation. This is how to restore health. With that in mind, let’s go over five reasons why your thyroid medication may not be working, based on the actual thyroid problem you might have:
1. Decreased thyroid receptor sensitivity
Every cell of your body is lined with what is called a bilipid membrane. This membrane is made of saturated fat and cholesterol and your health depends on this membrane’s integrity and functionality. Receptor sites on the membrane act as communicators with hormones, but the presence of cellular inflammation can cause a rigidity of the cell membrane and a “dulling,” or resistance, of the receptor sites. (36) Your body may be producing enough thyroid hormone or you may be on the right dose of thyroid hormone drug, but if your cells aren’t communicating with the hormone, your symptoms will persist because your body cannot communicate with those hormones.
2. Decreased thyroid hormone conversion.
Inflammation can cause other problems as well. It can decrease the body’s ability to convert the inactive thyroid hormone, T4, to the biologically active and usable form, T3. (37) This hormone conversion happens primarily in the liver and your gut and is essential for your body to utilize thyroid hormone. When that conversion fails, your symptoms will persist, even in the presence of thyroid medication, which (as I mentioned above) is typically in the form of T4 and needs to be converted to T3, just like the hormones your own body makes.
3. High reverse T3 levels.
When your body is under chronic stress, it can produce higher levels of reverse T3, (38) which is an inactive form of the thyroid hormone. Reverse T3 can’t be converted into T3, so it basically takes up space and interferes with the healthy production and conversion of regular T3 – another situation where the problem isn’t a deficiency in thyroid hormone, but a conversion problem caused by chronic stress and inflammation.
4. Decreased brain-thyroid communication.
Your thyroid doesn’t act on its own. It receives directions from your brain, specifically the hypothalamus and pituitary glands. Think of your thyroid as an employee of the brain, only doing what the brain tells it to do. This interconnected web of communication is called the hypothalamic-pituitary-thyroid (HPT) axis. (39) Chronic stress, autoimmune responses, and inflammation in any of these areas can negatively impact these communication lines, so thyroid hormone production could be impacted by a problem in the hypothalamus or pituitary glands, when the thyroid gland is fine.
5. Selenium deficiency.
Although relatively rare in adults, a selenium deficiency can sometimes result in people with chronic inflammation, such as may occur with gastrointestinal disease. (40) Selenium is an essential micronutrient that plays an important role in thyroid hormone conversion and overall function. Dietary sources include nuts, meats, fish, and eggs.
What’s the take-away?
The short answer to the question of why your thyroid medication isn’t working lies in the one common component in all the various ways thyroid dysfunction can happen: Inflammation. Inflammation is the common link between all chronic diseases, so assessing and addressing your own levels of chronic inflammation is an essential first step to restoring thyroid health. A comprehensive health history and lab tests can determine both your levels and underlying sources of inflammation, such as chronic infection, toxicity, food intolerances, autoimmune response, or a combination of these. This is a beginning because without reducing inflammation, optimal health is not possible.
Nutrients For Healthy Thyroid Hormones
Here is my guide to the essential aspects of thyroid function and how to support each through nutrition.
TSH
Thyroid-stimulating hormone, or TSH, is released from your pituitary gland to communicate with your thyroid. For healthy, happy TSH, you need four things:
1. Protein
Great bioavailable sources of protein are wild-caught fish, grass-fed beef, and blue and green algae.
2. Vitamin B12
A great source of B12 is grass-fed beef. Additionally, B12 can be found (41) in egg yolk, salmon, and organ meats such as liver.
3. Magnesium
Dark, leafy greens like spinach and kale are good sources, as well as nuts and seeds (preferably soaked in water for a few hours then dried before eating).
4. Zinc
Grass-fed beef is the highest food source. Shellfish like lobster, mussels, and oysters also contain zinc. Nuts and seeds are good plant-based options.
T4
T4 is another thyroid hormone that is typically inactive in the body and has to be converted to T3 to be usable, except in your brain, which needs straight-up T4 to work optimally. (42) For T4 production you need three essential nutrients:
1. Iodine
The “4” of T4 represents four iodine molecules. The best iodine-rich foods are sea vegetables like dulse, kombu, nori, arame, and kelp.
2. Vitamin B2
The best sources for B2 are grass-fed liver and lamb. Mushrooms and greens are decent plant sources.
3. Vitamin C
Your thyroid needs to draw iodine in to make T4 through what’s called a symporter, which requires (43) both vitamin B2 and vitamin C. The symporter won’t work (44) unless you have these two nutrients! Oranges and red peppers are the best foods to get your vitamin C.
T3
This is the more active, usable form of thyroid hormone, which is converted from T4. Think of T3 as your body’s gasoline.
1. Selenium
Without selenium we won’t convert T4 to T3, and we make more of an unusable thyroid hormone that can actually block (45) thyroid function. The best way to get your selenium is Brazil nuts. I suggest getting your selenium levels tested and eating two to four Brazil nuts (soaked in water for a few hours before eating) each day to get all the selenium you need.
Thyroid Receptor Site
In addition to the necessary thyroid hormones, you need healthy receptor sites for your hormones to work. Like a lock and key, hormones and their receptor site need to line up and function properly. To keep your thyroid receptor sites in tip-top shape, you need:
1. Vitamin A
Low levels of vitamin A and vitamin D can stop T3 from activating. Grass-fed liver and tuna are the highest sources of true vitamin A, which is only found in animal meat. Sweet potatoes and carrots are good sources for the plant-based vitamin A precursor known as beta-carotene.
2. Vitamin D
Responsible for over (46) 200 genetic pathways, this sunshine vitamin is super important, especially when it comes to supporting thyroid hormone receptor sites. The best food sources of vitamin D are fatty fish like salmon, beef liver, and egg yolks. Even more importantly: Get out in the sun whenever you can!
You can use food as medicine to support your thyroid function.
Now that we understand what your thyroid hormones need to thrive, let’s put it into action! Here’s a sample meal plan to get all those nutrients into your day:
Breakfast: Thyroid Booster Smoothie
Lunch: Wild-Caught Salmon with avocado sauce + Brussels sprouts
Dinner: Probiotic Superfood Burger with greens + asparagus
As one of the first functional medicine telehealth clinics in the world, we provide webcam health consultations for people around the globe.
Read Next: Can You Simultaneously Detox Your Body And Balance Your Hormones Naturally?
Photo: Stocksy
Start Your Health Journey Today
FUNCTIONAL MEDICINE CONSULTATIONS FOR PEOPLE AROUND THE WORLD
References:
- Nobuyuki Amino 4 Autoimmunity and hypothyroidism Bailiére's Clinical Endocrinology and Metabolism Volume 2, Issue 3 August 1988. doi:10.1016/S0950-351X(88)80055-7
- van Rijn LE, Pop VJ, Williams GR. Low bone mineral density is related to high physiological levels of free thyroxine in peri-menopausal women. Eur J Endocrinol. 2014;170(3):461‐468. Published 2014 Feb 7. doi:10.1530/EJE-13-0769
- Yaylali O, Kirac S, Yilmaz M, et al. Does hypothyroidism affect gastrointestinal motility?. Gastroenterol Res Pract. 2009;2009:529802. doi:10.1155/2009/529802
- NHS “Erectile dysfunction (impotence)” 16 August 2017 https://www.nhs.uk/conditions/erection-problems-erectile-dysfunction/
- Kalra S, Unnikrishnan AG, Sahay R. The hypoglycemic side of hypothyroidism. Indian J Endocrinol Metab. 2014;18(1):1‐3. doi:10.4103/2230-8210.126517
- Abrams JJ, Grundy SM. Cholesterol metabolism in hypothyroidism and hyperthyroidism in man. J Lipid Res. 1981;22(2):323‐338.
- CJ Gardner, P Richardson, et al. Hypothyroidism in a patient with non-alcoholic fatty liver disease BMJ 2011; 342 doi: https://doi.org/10.1136/bmj.c7199
- Sintzel F, Mallaret M, Bougerol T. Potentialisation par les hormones thyroïdiennes des traitements tricycliques et sérotoninergiques dans les dépressions résistantes [Potentializing of tricyclics and serotoninergics by thyroid hormones in resistant depressive disorders]. Encephale. 2004;30(3):267‐275. doi:10.1016/s0013-7006(04)95439-5
- Berent D, Zboralski K, Orzechowska A, Gałecki P. Thyroid hormones associated with depression severity and clinical outcome in patients with major depressive disorder. Mol Biol Rep. 2014;41(4):2419‐2425. doi:10.1007/s11033-014-3097-6
- Brănişteanu DE, Dimitriu A, Vieriu M, et al. Cutaneous manifestations associated with thyroid disease. Rev Med Chir Soc Med Nat Iasi. 2014;118(4):953‐958.
- B. Winsa, MD, A. Karlsson, MD et al. Stressful life events and Graves' disease The Lancet VOLUME 338, ISSUE 8781, P1475-1479, DECEMBER 14, 1991 doi: https://doi.org/10.1016/0140-6736(91)92298-G
- Matos‐Santos, A., Nobre, E.L., Costa, J.G.E., Nogueira, P.J., Macedo, A., Galvão‐Teles, A. and De Castro, J.J. (2001), Relationship between the number and impact of stressful life events and the onset of Graves' disease and toxic nodular goitre★. Clinical Endocrinology, 55: 15-19. doi:10.1046/j.1365-2265.2001.01332.x
- Sategna-Guidetti C, Bruno M, Mazza E, et al. Autoimmune thyroid diseases and coeliac disease. Eur J Gastroenterol Hepatol. 1998;10(11):927‐931. doi:10.1097/00042737-199811000-00005
- Mainardi E, Montanelli A, Dotti M, Nano R, Moscato G. Thyroid-related autoantibodies and celiac disease: a role for a gluten-free diet?. J Clin Gastroenterol. 2002;35(3):245‐248. doi:10.1097/00004836-200209000-00009
- Roland Gärtner, Barbara C. H. Gasnier, Johannes W. Dietrich, Bjarne Krebs, Matthias W. A. Angstwurm, Selenium Supplementation in Patients with Autoimmune Thyroiditis Decreases Thyroid Peroxidase Antibodies Concentrations, The Journal of Clinical Endocrinology & Metabolism, Volume 87, Issue 4, 1 April 2002, Pages 1687–1691, https://doi.org/10.1210/jcem.87.4.8421
- Baeke F, Takiishi T, Korf H, Gysemans C, Mathieu C. Vitamin D: modulator of the immune system. Curr Opin Pharmacol. 2010;10(4):482‐496. doi:10.1016/j.coph.2010.04.001
- Arrieta MC, Bistritz L, Meddings JB. Alterations in intestinal permeability. Gut. 2006;55(10):1512‐1520. doi:10.1136/gut.2005.085373
- Langer P, Kocan A, Tajtaková M, et al. Fish from industrially polluted freshwater as the main source of organochlorinated pollutants and increased frequency of thyroid disorders and dysglycemia. Chemosphere. 2007;67(9):S379‐S385. doi:10.1016/j.chemosphere.2006.05.132
- Martin I. Surks, M.D., and Rubens Sievert, M.D. Drugs and Thyroid Function N Engl J Med 1995; 333:1688-1694 DOI: 10.1056/NEJM199512213332507
- Boukis MA, Koutras DA, Souvatzoglou A, Evangelopoulou A, Vrontakis M, Moulopoulos SD. Thyroid hormone and immunological studies in endemic goiter. J Clin Endocrinol Metab. 1983;57(4):859‐862. doi:10.1210/jcem-57-4-859
- Tomer Y, Huber A. The etiology of autoimmune thyroid disease: a story of genes and environment. J Autoimmun. 2009;32(3-4):231‐239. doi:10.1016/j.jaut.2009.02.007
- Vestergaard P, Rejnmark L, Weeke J, et al. Smoking as a risk factor for Graves' disease, toxic nodular goiter, and autoimmune hypothyroidism. Thyroid. 2002;12(1):69‐75. doi:10.1089/105072502753451995
- Wajner SM, Goemann IM, Bueno AL, Larsen PR, Maia AL. IL-6 promotes nonthyroidal illness syndrome by blocking thyroxine activation while promoting thyroid hormone inactivation in human cells. J Clin Invest. 2011;121(5):1834‐1845. doi:10.1172/JCI44678
- Farhangi MA, Keshavarz SA, Eshraghian M, Ostadrahimi A, Saboor-Yaraghi AA. The effect of vitamin A supplementation on thyroid function in premenopausal women. J Am Coll Nutr. 2012;31(4):268‐274. doi:10.1080/07315724.2012.10720431
- Hedrén E, Diaz V, Svanberg U. Estimation of carotenoid accessibility from carrots determined by an in vitro digestion method. Eur J Clin Nutr. 2002;56(5):425‐430. doi:10.1038/sj.ejcn.1601329
- Olivieri O, Girelli D, Stanzial AM, Rossi L, Bassi A, Corrocher R. Selenium, zinc, and thyroid hormones in healthy subjects: low T3/T4 ratio in the elderly is related to impaired selenium status. Biol Trace Elem Res. 1996;51(1):31‐41. doi:10.1007/BF02790145
- Drutel A, Archambeaud F, Caron P. Selenium and the thyroid gland: more good news for clinicians. Clin Endocrinol (Oxf). 2013;78(2):155‐164. doi:10.1111/cen.12066
- Zimmermann MB, Köhrle J. The impact of iron and selenium deficiencies on iodine and thyroid metabolism: biochemistry and relevance to public health. Thyroid. 2002;12(10):867‐878. doi:10.1089/105072502761016494
- Jain RB. Thyroid function and serum copper, selenium, and zinc in general U.S. population. Biol Trace Elem Res. 2014;159(1-3):87‐98. doi:10.1007/s12011-014-9992-9
- Abdel-Dayem, M.M., Elgendy, M.S. Effects of chronic estradiol treatment on the thyroid gland structure and function of ovariectomized rats. BMC Res Notes 2, 173 (2009). https://doi.org/10.1186/1756-0500-2-173
- Understanding Local Control of Thyroid Hormones: (Deiodinases Function and Activity) NAHIS https://www.nahypothyroidism.org/deiodinases/
- Nobuyuki Amino 4 Autoimmunity and hypothyroidism Baillière's Clinical Endocrinology and Metabolism Volume 2, Issue 3, August 1988, Pages 591-617 doi: https://doi.org/10.1016/S0950-351X(88)80055-7
- Yang, J., Yang, X. & Li, M. Baicalin, a natural compound, promotes regulatory T cell differentiation. BMC Complement Altern Med 12, 64 (2012). https://doi.org/10.1186/1472-6882-12-64
- Asvold BO, Bjøro T, Nilsen TI, Gunnell D, Vatten LJ. Thyrotropin levels and risk of fatal coronary heart disease: the HUNT study. Arch Intern Med. 2008;168(8):855‐860. doi:10.1001/archinte.168.8.855
- Anthony Martin Gerdes and Giorgio Iervasi Thyroid Replacement Therapy and Heart Failure Circulation 2010;122:385–393 https://doi.org/10.1161/CIRCULATIONAHA.109.917922
- Hiroaki Kimura and Patrizio Caturegli Chemokine Orchestration of Autoimmune Thyroiditis Thyroid 2007 17:10, 1005-1011 https://doi.org/10.1089/thy.2007.0267
- Molnár I, Balázs C, Szegedi G, Sipka S. Inhibition of type 2,5'-deiodinase by tumor necrosis factor alpha, interleukin-6 and interferon gamma in human thyroid tissue. Immunol Lett. 2002;80(1):3‐7. doi:10.1016/s0165-2478(01)00301-7
- Kjellman BF, Ljunggren JG, Beck-Friis J, Wetterberg L. Reverse T3 levels in affective disorders. Psychiatry Res. 1983;10(1):1‐9. doi:10.1016/0165-1781(83)90022-7
- Mebis L, van den Berghe G. The hypothalamus-pituitary-thyroid axis in critical illness. Neth J Med. 2009;67(10):332‐340.
- Rannem T, Ladefoged K, Hylander E, Hegnhøj J, Staun M. Selenium depletion in patients with gastrointestinal diseases: are there any predictive factors?. Scand J Gastroenterol. 1998;33(10):1057‐1061. doi:10.1080/003655298750026750
- Vitamin B12 Health Sheet NIH March 30, 2020 https://ods.od.nih.gov/factsheets/VitaminB12-HealthProfessional/
- Schroeder AC, Privalsky ML. Thyroid hormones, t3 and t4, in the brain. Front Endocrinol (Lausanne). 2014;5:40. Published 2014 Mar 31. doi:10.3389/fendo.2014.00040
- Moncayo R, Kroiss A, Oberwinkler M, et al. The role of selenium, vitamin C, and zinc in benign thyroid diseases and of selenium in malignant thyroid diseases: Low selenium levels are found in subacute and silent thyroiditis and in papillary and follicular carcinoma. BMC Endocr Disord. 2008;8:2. Published 2008 Jan 25. doi:10.1186/1472-6823-8-2
- Guy E. Abraham, M.D. (1) and David Brownstein, M.D. PUB. #11: Evidence that the administration of vitamin C improves a defective cellular transport mechanism for iodine: A case report. The Original Internist. 2005; 12(3):125-130. https://www.optimox.com/content/Iodine%20Research%20Resources/IOD11.pdf
- Anna J Duffield, Christine D Thomson, Kristina E Hill, Sheila Williams, An estimation of selenium requirements for New Zealanders, The American Journal of Clinical Nutrition, Volume 70, Issue 5, November 1999, Pages 896–903, https://doi.org/10.1093/ajcn/70.5.896
- Hossein-nezhad A, Spira A, Holick MF. Influence of vitamin D status and vitamin D3 supplementation on genome wide expression of white blood cells: a randomized double-blind clinical trial. PLoS One. 2013;8(3):e58725. doi:10.1371/journal.pone.0058725
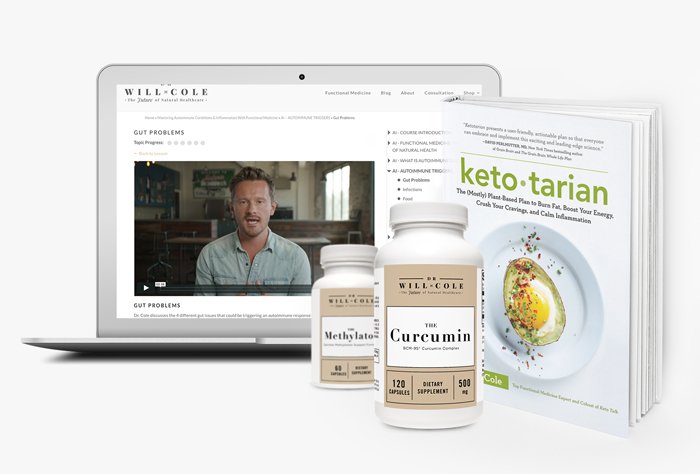
View More At Our Store
Purchase personally curated supplements
and Dr. Will Cole’s books!
The information on this website has not been evaluated by the Food & Drug Administration or any other medical body. We do not aim to diagnose, treat, cure or prevent any illness or disease. Information is shared for educational purposes only. You must consult your doctor before acting on any content on this website, especially if you are pregnant, nursing, taking medication, or have a medical condition.
Our articles may include products that have been independently chosen and recommended by Dr. Will Cole and our editors. If you purchase something mentioned in this article, we may earn a small commission.

BY DR. WILL COLE
Dr. Will Cole, DNM, IFMCP, DC is a leading functional medicine expert who consults people around the globe, starting one of the first functional medicine telehealth centers in the world. Named one of the top 50 functional and integrative doctors in the nation, Dr. Will Cole provides a functional medicine approach for thyroid issues, autoimmune conditions, hormonal imbalances, digestive disorders, and brain problems. He is also the host of the popular The Art of Being Well podcast and the New York Times bestselling author of Intuitive Fasting, Ketotarian, Gut Feelings, and The Inflammation Spectrum.

Gut Feelings
Healing The Shame-Fueled Relationship
Between What You Eat And How You Feel


