How To Know If You Need An Antibiotic + Exactly What To Do About It

Antibiotics are a type of medication that are prescribed to patients in order to kill bacterial infections. They are given more than 154 million times a year and the CDC states that close to 30 percent of the time (1) it is unnecessary. Some reports even say that the number is actually closer to 50 percent. That is a statistic that should make us all take pause since there are many consequences that go along with taking antibiotics, especially if they are unneeded.
For example, an overuse of antibiotics in our society has caused a rapid rise of antibiotic-resistant infections such as MRSA. Not to mention the many direct side effects (2) of antibiotic use. About 14,000 Americans die every year from diarrhea caused by antibiotics and many others have to live with permanent damage to their nerves, tendons, and skin. These shocking facts should have us questioning: what are these antibiotics doing to our immune systems?
A large part – close to 75 percent – of your immune system resides in your microbiome. Antibiotics are known to damage this collection of bacteria in your gut which is vital in maintaining optimal health. The antibiotic ciprofloxacin, for example, has been shown to reduce (3) the bacterial diversity of your microbiome by about one-third. Even though most of the bacterial diversity recovered after the round of antibiotics ended, some bacterial strains still hadn’t recovered six months later.
Article continues below
Make Your Life a Cleanse
SUBSCRIBER-ONLY GUIDES FOR GUT HEALTH, VIBRANT ENERGY, HEALTHY FOOD & CLEAN ALCOHOL
Get FREE access to these + giveaways, recipes, & discount codes in personal emails from Dr. Will Cole.
When antibiotics can actually be helpful (and even lifesaving)
Although there are many dangers of overusing antibiotics, it’s important to recognize that there are times when antibiotics have actually saved lives. Proper antibiotic use is all about using discretion to decide on when they are needed and when they are not. So, when are some instances when antibiotics can be a good course of action? If infection is a concern, seeing a doctor can help determine the nature of your illness to find out if it can be threatening. There are two major categories of infection:
1. Viral infections
The common cold and the flu (influenza) are both upper respiratory infections that are caused by viruses, not bacteria. In fact, sinus infections and eye infections like pinkeye are also almost always caused by viruses. Since antibiotics are designed to only kill bacteria, knowing what type of infection you have can narrow down whether or not an antibiotic will even be effective.
2. Bacterial infections
Once you know that your illness is bacterial in nature and not viral, it is still important to remember that there are a lot of different kinds of bacterial infections which should be evaluated on a case-by-case basis with the help of your doctor. An ear infection is one example of an infection that in general, can resolve itself after a few days. However, urinary tract infections can sometimes need the help of antibiotics if not also resolved after a few days. Skin infections as well – ones that include red and inflamed areas – can benefit from the use of antibiotics.
What about natural antibiotics?
Luckily there are many natural antibiotics that can either amplify the effect of pharmaceutical options or can be used on their own. Oregano oil is one of my favorites and has been shown to be effective (4) in fighting staph infections when used alongside monolaurin – a by-product of coconut oil, which also has its own antibacterial properties.
How to support your body when taking antibiotics
If you have decided that your bacterial infection does need the support of a prescribed antibiotic there is still a lot you can do to give your body the TLC it needs while you are taking this medication:
1. Antioxidants
Antioxidants fight free radical compounds that contribute to making us sick. Food should ultimately be the primary source of our antioxidants but for times like this when your immune system needs an extra boost I turn to:
- N-acetylcysteine (NAC): This powerful antioxidant is a precursor to one of your body’s most vital antioxidants – glutathione. NAC has also been shown to have natural antibiotic properties by beneficially regulating biofilms. This bacterial protective slime can be the cause (5) of ongoing bacterial infections. NAC is a key ingredient in my blend Protect.
- Pterostilbene: Blueberries, almonds, and grape leaves are all good sources of this antioxidant. (6) Pterostilbene is chemically similar to resveratrol but has been found to be even more potent. Research has shown that it is in fact, four times more bioavailable than resveratrol. It can also increase the molecule NAD (nicotinamide adenine dinucleotide) which has intense anti-aging effects.
- Curcumin and Turmerone: No antioxidant list is complete without turmeric. Curcuminoids and turmerones are active compounds found in this spice that are able to reduce the negative effects of antibiotics.
- Andrographis: I often recommend this herb to my patients who are taking antibiotics as a natural antibacterial (7) viral agent.
2. Probiotics
While many people can benefit from taking quality probiotics, it is especially important for those taking antibiotics. Studies have shown that taking a probiotic in conjunction with your antibioitics – while seemingly contradictory – can reduce some of the side effects.
3. Bone broth
Bone broth is probably my favorite food medicine to nourish the primary home of your immune system – the gut. You can either make your own or purchase it already premade. Bare Bones and Kettle & Fire are my go-to brands since they use the highest quality ingredients. By being packaged frozen, all the real food goodness is preserved unlike most other shelf-stable carton bone broths.
As one of the first functional medicine telehealth clinics in the world, we provide webcam health consultations for people around the globe.
Photo: Stocksy
Start Your Health Journey Today
FUNCTIONAL MEDICINE CONSULTATIONS FOR PEOPLE AROUND THE WORLD
References:
- CDC: 1 in 3 antibiotic prescriptions unnecessary CDC May 3, 2016. https://www.cdc.gov/media/releases/2016/p0503-unnecessary-prescriptions.html
- Blaser, M. Stop the killing of beneficial bacteria. Nature 476, 393–394 (2011). https://doi.org/10.1038/476393a
- Dethlefsen L, Huse S, Sogin ML, Relman DA. The pervasive effects of an antibiotic on the human gut microbiota, as revealed by deep 16S rRNA sequencing. PLoS Biol. 2008;6(11):e280. doi:10.1371/journal.pbio.0060280
- Harry G. Preuss, Bobby Echard, Azad Dadgar, Nadeem Talpur, Vijaya Manohar, Mary Enig, Debasis Bagchi & Cass Ingram (2005) Effects of Essential Oils and Monolaurin on Staphylococcus aureus: In Vitro and In Vivo Studies, Toxicology Mechanisms and Methods, 15:4, 279-285, DOI: 10.1080/15376520590968833
- Dinicola S, De Grazia S, Carlomagno G, Pintucci JP. N-acetylcysteine as powerful molecule to destroy bacterial biofilms. A systematic review. Eur Rev Med Pharmacol Sci. 2014;18(19):2942‐2948.
- Denise McCormac and David McFadden A Review of Pterostilbene Antioxidant Activity and Disease Modification Oxidative Medicine and Cellular Longevity 2013. doi:10.1155/2013/575482
- Arifullah M, Namsa ND, Mandal M, Chiruvella KK, Vikrama P, Gopal GR. Evaluation of anti-bacterial and anti-oxidant potential of andrographolide and echiodinin isolated from callus culture of Andrographis paniculata Nees. Asian Pac J Trop Biomed. 2013;3(8):604‐610. doi:10.1016/S2221-1691(13)60123-9
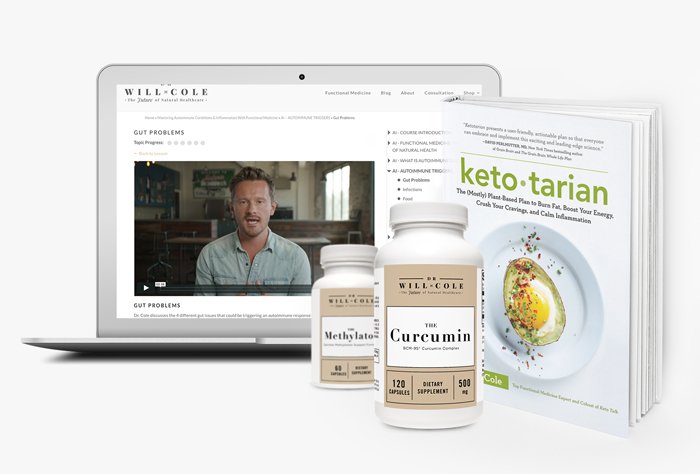
View More At Our Store
Purchase personally curated supplements
and Dr. Will Cole’s books!
The information on this website has not been evaluated by the Food & Drug Administration or any other medical body. We do not aim to diagnose, treat, cure or prevent any illness or disease. Information is shared for educational purposes only. You must consult your doctor before acting on any content on this website, especially if you are pregnant, nursing, taking medication, or have a medical condition.
Our articles may include products that have been independently chosen and recommended by Dr. Will Cole and our editors. If you purchase something mentioned in this article, we may earn a small commission.

BY DR. WILL COLE
Dr. Will Cole, DNM, IFMCP, DC is a leading functional medicine expert who consults people around the globe, starting one of the first functional medicine telehealth centers in the world. Named one of the top 50 functional and integrative doctors in the nation, Dr. Will Cole provides a functional medicine approach for thyroid issues, autoimmune conditions, hormonal imbalances, digestive disorders, and brain problems. He is also the host of the popular The Art of Being Well podcast and the New York Times bestselling author of Intuitive Fasting, Ketotarian, Gut Feelings, and The Inflammation Spectrum.

Gut Feelings
Healing The Shame-Fueled Relationship
Between What You Eat And How You Feel


