The Negative Effects Of Gluten + The Best Way To Go Gluten-Free

Celiac disease is a real autoimmune disease that requires giving up gluten for life. But what about all the other people who don’t have celiac disease and claim they are “gluten intolerant”? Is that really a thing, or is it just a bunch of hype, or the latest dietary fad, like the low-fat craze of the 1980s that turned out to have little or no merit?
“Gluten intolerance” may just be one of the most controversial health terms these days. If you do a little research, you may discover that according to estimates, approximately 18 million Americans have a “gluten sensitivity.”
The growing awareness of the very existence of gluten – a protein found in certain grains including wheat, rye, barley, and spelt – has born an endless parade of gluten-free everything. Gluten-free cookies, gluten-free cereal, gluten-free baking mixes, gluten-free bread, gluten-free crackers – you could probably find gluten-free gluten if you searched hard enough!
I’m kidding, of course, but seriously, what’s the deal? Is gluten something you really should avoid, or are you wasting your money and missing out on a practically ubiquitous protein? The subject is quite controversial, with passionate advocates on both sides of the argument, so let’s take a closer look, and see what science has to say on the subject.
Article continues below
Make Your Life a Cleanse
SUBSCRIBER-ONLY GUIDES FOR GUT HEALTH, VIBRANT ENERGY, HEALTHY FOOD & CLEAN ALCOHOL
Get FREE access to these + giveaways, recipes, & discount codes in personal emails from Dr. Will Cole.
Is gluten intolerance real?
Not everyone agrees yet, but an increasing number of doctors and scientists are saying yes. One trial (1) published in Clinical Gastroenterology and Hepatology studied people who thought gluten was causing them digestive problems. The gold standard for research is something called a randomized, double-blind, placebo-controlled, crossover trial, and gluten was put to this rigorous test.
For one week, participants were given either a small amount of gluten or a placeo pill of rice starch. After only one week, those who were taking the gluten pills reported a significant increase in symptoms compared to those who took gluten-free placebo pills.
Another recent randomized control trial shared similar findings. (2) These studies are good evidence that some people do experience uncomfortable side effects after eating gluten. More research is ongoing, and I expect that as the concept of gluten intolerance continues to gain credence, we will see even more reputable research legitimizing this condition.
Is gluten intolerance an autoimmune condition?
To understand gluten intolerance, we need to understand autoimmune conditions. Many people think when we talk about gluten intolerance we are referring to the autoimmune condition celiac disease. Yes, celiac is an autoimmune disease, but it is the extreme end of a broader gluten-intolerance spectrum. (3)
You can be on the autoimmune-inflammation spectrum without having celiac disease, and that can result in gluten intolerance, or what doctors sometimes call non-celiac gluten sensitivity (NCGS). You may not have tests that come back saying you have an autoimmune disease, but I believe that gluten reactivity is a warning that you could eventually be headed in that direction if you don’t change your diet and health habits.
What are the symptoms of gluten intolerance?
People in the study experienced:
- abdominal bloating
- ulcers
- intestinal pain
But how do you know if you have it? The first thing to consider is whether you have any of the other classic symptoms of gluten intolerance that can often be overlooked, which include:
- Other autoimmune conditions besides celiac disease
- Other chronic health issues, such as Hashimoto’s, Crohn’s, or adrenal fatigue
- Skin eruptions in the form of eczema, cold sores, or acne
- Chronic unexplained fatigue
- Chronic unexplained joint pain (or rheumatoid arthritis, another autoimmune disease)
- Indigestion, bloating, gas, heartburn, or other uncomfortable symptoms that occur after eating
- Constipation
- Diarrhea
- Congestion during or after eating
- Unexplained anxiety, moodiness, or irritability
- Chronic headaches or migraines
- Brain fog
- Depression
- Anxiety
Can you test for gluten intolerance?
You can get tested for celiac disease, but assessing gluten tolerance is a little more difficult. Mention gluten, and a conventional doctor will likely get a simple alpha gliadin lab.
These tests do offer helpful but incomplete information:
- Gliadin, the protein component of gluten, has four different sub classifications: alpha, beta, gamma, and omega. The problem with the typical gliadin antibody test is that it only tests alpha gliadin. You could have a negative alpha gliadin antibody test but have a positive response against another form of gliadin. This quirk gives many the impression that gluten isn’t a problem for them, and they continue to feed their health problems with every meal.
- The anti-transglutaminase antibody test (4) is run to rule out celiac disease, the autoimmune disease, which is known for its severe reaction against gluten. If you have celiac disease, you certainly want to know this information. However, if this is the only test your doctor does, he or she may not be aware of the increasing amount of research (5) being done on non-celiac gluten sensitivity (NCGS). An estimated 18 million Americans (6) may have some form of gluten sensitivity or intolerance.
On top of all that, some people react to other aspects of wheat gluten – in fact, there are about 24 different qualities in wheat that can cause reactivity. More comprehensive labs could be incredibly helpful for someone who needs motivation to eliminate some or all grains, or for someone who has reintroduced grains into their diet but is still unsure whether grains are problematic for them.
So what tests should be done if you want to find out for sure if you have gluten intolerance? These are the main tests that I run on my patients to make a thorough diagnosis of gluten intolerance, or to rule it out and know to look elsewhere for the cause of symptoms:
1. Deamidated Gliadin
In many processed foods, wheat is put through a process of deamidation which makes it mix better with other ingredients. This chemical process also goes on in your intestines, which can further complicate the issue. Your body may tolerate every other form of gluten except deamidated gliadins. This test will help to clarify if that is the case for you.
2. Glutenin
Gliadin is not the only component to gluten. The other half of gluten is a compound called glutenin. This compound was once thought not to cause an inflammatory response in the body, but recent research (7) has shown that it actually can be a problem for some people. Looking at just part of gluten is like having only part of the pieces to a puzzle. This test completes the puzzle.
3. Gluteomorphins
Many of my patients feel worse when they first come off gluten. They’re probably detoxing off of gluteomorphins or gliadorphin. Gluteomorphins are opiate-like compounds that can make gluten a bit like an addictive drug. Coming off gluten can come with several days or weeks of irritability, brain fog, headaches, and lethargy. This test can clarify the reason for those symptoms.
4. Prodynorphin
Prodynorphins are necessary for your body to make endorphins. Their production can be suppressed (8) in someone with gluten sensitivity, and this test can illuminate that condition.
5. Wheat Germ Agglutinin
Wheat germ agglutinin (9) is the lectin component of wheat and can bind to nutrients to make them unusable in your body. They also can cause an immune response in your body, leading to chronic systemic inflammation. If this test is positive, you are reacting to a component of wheat that is not gluten but is nevertheless causing problems in your system.
6. Gluten Cross-Reactivity
This test can be the missing link for many people who are eating “gluten free” but are still having symptoms. When your body makes antibodies against gluten, those antibodies can also recognize proteins in other foods that have a similar structure. When you eat those foods, even though they don’t contain gluten, your body reacts (10) as though they do!
Some common gluten cross-reactive foods are rice, corn, soy, quinoa, and buckwheat. To get the whole story, as you can see, a comprehensive health history and testing is necessary and can be a life changer for many people whose symptoms remain undiagnosed. When we clinically investigate these underlying issues, that information allows us to create a customized health program for the individual.
The Health Effects Of Gluten
The Gluten-Thyroid Storm
Every cell in your body depends on your thyroid to make thyroid hormones the body can use, and these hormones impact your health in many different ways. If your thyroid hormones don’t function correctly, your health will suffer.
One common example of what can go wrong is low thyroid function, or hypothyroidism. Around 20 million Americans and 250 million people worldwide have this problem, and one in eight women will struggle with a thyroid problem in her lifetime. Add to that the fact that up to 90% of all thyroid problems are autoimmune in nature – the most common of which is Hashimoto’s.
Yet, there’s a 30% chance that the antibody test to diagnose Hashimoto’s will present an indecisive or false negative result, causing many Hashimoto’s cases to go undiagnosed for years. In other words, many people are walking around with a serious autoimmunity problem and don’t even know it.
Autoimmune diseases don’t just appear out of nowhere. They tend to happen on a spectrum, starting with very few symptoms and progressing until they are quite advanced and diagnosable. In my experience, the majority of low-thyroid problems are somewhere on this autoimmune spectrum, even before a conventional doctor can diagnose a disease such as Hashimoto’s. But wouldn’t you rather stop that gluten-thyroid storm before it causes too much damage to your health? To do this, we have to look at what triggers the immune system to attack the thyroid, rather than just treating symptoms and ignoring the cause.
When the immune system mistakenly attacks the thyroid gland, it is often a case of mistaken identity, and gluten is one of the main culprits. (11) Gluten is the protein found in wheat and some other grains, and when it passes through the gut lining and into the blood stream, the immune system will tag the “foreign invader” (gluten) with antibodies for destruction. This can cause a lot of damage to your body as it gets caught in this crossfire – and often times, it is the thyroid that gets mistaken for gluten, due to a similarity in how the molecules look to your immune system.
The Gluten-Brain Storm
Although just 1% of Americans have a diagnosis of celiac disease, it’s most likely vastly under-diagnosed. In fact, only 10% of people with the disease exhibit obvious GI symptoms, and research now suggests (12) that celiac disease can present itself strictly as a neurological problem.
In reality, celiac disease doesn’t exist in a vacuum, nor is it something you either have or don’t have. Instead, celiac disease is the extreme end of the gluten sensitivity-autoimmune spectrum. For example, the estimated 1 in 20 Americans living with what’s called non-celiac gluten sensitivity are likely somewhere in the middle of that spectrum, reacting to gluten but without having yet suffered the extreme small intestine destruction necessary for a celiac disease diagnosis.
We know that gluten has been shown to increase (13) levels of the protein zonulin in the gut, which leads to leaky gut syndrome due to its effects on the tight junctions of the intestinal lining. This gut permeability allows undigested food proteins and bacterial endotoxins to pass into the blood stream, activating an inflammatory-immune response in the body.
Elevated zonulin levels in the gut have also been linked to elevated zonulin levels in the brain. Translation: A leaky gut can lead to a leaky brain. Once the blood-brain barrier has been breached, your brain’s immune system – specifically its glial cells – can be activated. Glial cells can then cause an inflammatory cascade throughout the brain.
In other words, gluten is a sort of gateway food that could allow other foods to pass through the gut and brain lining, setting you on the autoimmune spectrum and on a course towards eventual disease.
So what’s the gluten verdict?
The bottom line is that, based on what science has discovered so far, some people do appear to have gluten intolerance, even when they do not have diagnosable celiac disease. But not everybody is sensitive to gluten. A recent study (14) in the journal Digestion found that 86 percent of people who thought they were gluten sensitive could actually tolerate gluten just fine. Symptoms they had interpreted as being gluten-related were likely related to some other aspect of wheat, or some other food or lifestyle issue.
We are all different, so there is no one-size-fits-all rule about gluten, or any other food, but when it comes to gluten, comprehensive testing is the best way to know for sure whether gluten is a problem for you.
6 Ways Grains Are Destroying Your Health
And it's not just gluten we have to worry about. We live in a grain-centric society. Most of the foods people buy in grocery stores are grain-based (just look in other people’s grocery carts), and grains have become the foundation of what people have on their plates: cereal or toast for breakfast, a sandwich for lunch, and a grain (rice, pasta, bread, etc.) as a side or even the main course at dinner. They’re the backbone of industrial farming, and a multibillion-dollar juggernaut in politics and policy. Grains are even the foundation of the famous food pyramid (or a huge slice of the new USDA MyPlate), which is the government’s official word on how the public should be eating.
However, the surprising truth is that for many people, grains are actually not the health powerhouse we have been led to believe. On the contrary. For many people, grains cause a lot of problems beyond just gluten. Here are seven compelling reasons to ditch grains and replace them with healthier, more nutrient dense alternatives:
1. Lectins
Lectins are another type of protein found in grains. These grain defense mechanisms made to keep insects from killing the grain plants also happen to be highly indigestible by the human body. Like gluten, lectins can wreak havoc on your gut, (15) leading to conditions like leaky gut syndrome. When your gut is damaged by this mild toxin, your body’s defense systems are compromised, causing inflammation. Lectins can also bind to insulin (16) and leptin (17) receptor sites, causing hormonal resistance patters, weight gain, and excessive hunger.
2. Enzyme inhibitors
Your body makes enzymes to break down and digest foods, but grains contain substances – alpha-amylase inhibitors and protease inhibitors – that inhibit the action of these enzymes, making the digestion of starches and proteins very difficult for your body.
3. Phytic acid
Phytates are anti-nutrients (18) that bind to minerals in your body and make them unusable, so just as enzyme inhibitors inhibit the enzymes you need to digest your food, phytates inhibit the absorption of minerals your body needs to get from foods. Mineral deficiencies like osteoporosis are perpetuated by the presence of phytates, which bind to minerals like calcium. The little nutrients that grains do offer are diminished by phytates, which make them unavailable for your body, so they offer little benefit.
4. Saponins
These anti-nutrients are high in pseudo-grains like quinoa, which are popular in the health community. Saponins can damage your gut, leading to increased gut permeability, which can contribute to inflammation and chronic conditions.
5. Amylose
That pasta or bread may not taste sweet, but grains are high in naturally occurring sugars like amylose. These sugars can overwhelm your body, causing blood sugar spikes that trigger insulin spikes, leading to excessive fat storage. This hormonal hurricane can lead to insulin resistance, high blood sugar, high triglycerides, and inflammation, all hallmarks of metabolic syndrome and diabetes.
6. Omega-6 fatty acids
Fats are essential for optimal health and we all need a balance of different kinds of fatty acids for optimal health. However, grains are high in polyunsaturated omega-6 fats, which are highly inflammatory when out of balance with omega-3 fats (such as those in cold-water fish and flax seed). This fat imbalance is not only found in grains but in the oils made from many plants, especially industrial oils like canola, corn, vegetable, and soybean oils. Combine grains and industrial oils (as is common in many processed foods) and you have a recipe for chronic systemic inflammation.
In addition to these six very good reasons to reduce or eliminate grain from your diet entirely, it is also important to remember that grains have changed dramatically from what they were in the past due to centuries of cross-breeding, hybridization, and genetic modification that has chemically altered grains, even from what they were a few decades ago.
Are there any good reasons to eat grains? Two common arguments are that grains are a good source of fiber, and that they are a good source of nutrients. But plenty of other less problematic foods also contain fiber and nutrients, such as vegetables and fruit. These whole plant foods are usually even more nutrient-dense, come with antioxidants, and don’t generally offend the gut, brain, immune system, or hormones.
Gluten-Free Flour Alternatives
Fortunately, you can have your cake (or cookies, or toast, or pasta) and eat it too, even if you are gluten-free and want to eat a nutrient-dense, healthful diet. If optimal health is your goal, consider which foods are the most nutrient-dense, have the most bioavailable nutrients, and cause the least amount of stress to your system. There are three types of flour that check all these boxes. They are nutrient-dense, gluten-free, and you can use them to make some of your old favorites (just take it easy on the sweetener). Here are my favorite gluten-free flours that are not junk food, that you can use when you bake:
1. Coconut flour
When coconut is finely ground into a flour, it still contains the nutritional components of the coconut, especially lauric acid, a healthful saturated fat that’s essential to your immune system function. Healthy saturated fats are critical for cellular health as well as glowing skin and thyroid health.
Because coconut flour comes from the meat of dried coconut, it is also a good source of clean protein and fiber, so it aids in healthy digestion and promotes gut health by providing a good food source for beneficial bacteria in your microbiome.
2. Almond flour
Best when made from organic almonds, almond flour contains valuable monounsaturated fats that can decrease the risk of heart disease. Almond flour is also abundant in the antioxidant vitamin E, magnesium, and potassium, all essential for building and maintain health.
3. Hazelnut flour
This nut flour is less known but is a great choice because of its high protein content. Hazelnut flour also boasts high levels of the B vitamin folate, which is important for cell health and brain development. Finally, hazelnut flour also has the highest proanthocyanidin content of any tree nut. These helpful compounds may help reduce the risk of blood clotting and urinary tract infections.
As with any food, what works for one person may not be the best for the next, as each of us has our own tolerances and some people are allergic to nuts or coconut. However, if these foods work for you and you have banished gluten from your life, these three flours are great alternatives. To improve your health even further, consider that my passion is to design health programs tailored to the individual, navigating them along a path of maximized health.
The Biggest Mistakes Made When Going Gluten-Free
The gluten-free industry is only expected to grow, achieving an astonishing $4.89 billion dollars by 2021, with a Monash University survey (19) finding that 78 percent of people who purchase gluten-free products say they do so for some sort of health reason.
Talking with patients from around the world in my functional medicine practice, I find that most have dabbled with a little “gluten-free,” and this is something I encourage, since research is indeed pointing to the fact that gluten is a likely trigger for both inflammation and autoimmune problems.
Yet, while 2.7 million (20) Americans (and millions more worldwide) either avoid gluten or know someone who does, misconceptions and misapplication of a gluten-free diet remain common. Don’t fall prey to these top mistakes I see people make when they decide to go gluten-free:
1. They quit too soon
A few weeks or a mere month of going gluten-free won’t, for many people, make enough of a difference. For example, the inflammatory effects (21) of gluten were shown to last up to six months in people with autoimmune thyroid problems, and I have found that gut problems like leaky gut syndrme can often take over a year to fully heal after gluten is removed from the diet. In other words, a chronic health problem that has taken years to become what it is today isn’t going to go away in three weeks. Give your gluten-free diet more time to work.
2. They don’t get complete gluten-sensitivity labs
If you are thinking about making the effort to go gluten-free (and in this wheat-happy culture, it is an effort), you will be more motivated if you know for sure it is the right move for you. Most people don’t realize that there are about 24 different properties in modern wheat that can cause sensitivity and reactions.
Make sure to work with a functional medicine practitioner to have the above comprehensive labs done.
3. They go gluten-free….for the most part
If you decide to go gluten-free, eating “a little bit” of gluten is like being “a little bit” pregnant – it’s an all-or-nothing proposition, folks. Simply cutting back won’t be effective or instructive. Normally, I suggest eliminating gluten entirely for at least 60 days before reintroducing to see if you react.
4. They eat too many gluten-free processed and inflammatory foods
Just because something is labeled gluten-free doesn’t mean it’s nutritious. Pure sugar, highly processed white rice flour and even high fructose corn syrup are all gluten-free, but they certainly aren’t good for you. These are some of the top contributors I see many people still eating even when going gluten-free.
- Soy
Soy products used to be all the rage in the health community, but this cheap and ubiquitous gluten-free food is high in phytoestrogens which can cause distress in the body and disruption to hormonal balance.
- Sugar
Just like fat-free foods, gluten-free foods can be loaded with added sugars. It’s no secret that refined sugars are anything but healthy. Just check the sugar content on that box of gluten-free cookies or gluten-free cake mix!
- Vegetable and industrial seed oils
Vegetable oil, canola oil, safflower oil, corn oil, and sunflower oil are cheap, highly processed, and used in just about all boxed foods, including ones marketed “gluten-free.” These oils are high in omega-6 polyunsaturated fatty acids (PUFAs) and can contribute to inflammation.
A healthy gluten-free diet is full of nutrient-dense and anti-inflammatory healthy fats, proteins, and organic plant-based foods.
5. They still eat cross-reactive foods
If you’ve gone gluten-free and initially felt better but then hit a plateau, cross-reactivity may be the culprit. Labs can be done that test for foods that do not contain gluten but that the body could be reading as gluten due to similar protein molecules – a bit like a case of mistaken identity!
6. They assume that a gluten-free diet will cure all of their problems
Going gluten-free can be a piece of your health puzzle, but it’s rarely a panacea. The human body is complex, and anyone suffering from inflammation likely requires multiple avenues of healing. Other issues like histamine intolerance and FODMAP intolerance are often overshadowed by gluten’s popularity, but also need to be addressed for optimal health.
As one of the first functional medicine telehealth clinics in the world, we provide webcam health consultations for people around the globe.
Photo: Stocksy
Read Next: 12 Of The Most Common Food Intolerances
Start Your Health Journey Today
FUNCTIONAL MEDICINE CONSULTATIONS FOR PEOPLE AROUND THE WORLD
References:
- Di Sabatino A, Volta U, Salvatore C, et al. Small Amounts of Gluten in Subjects With Suspected Nonceliac Gluten Sensitivity: A Randomized, Double-Blind, Placebo-Controlled, Cross-Over Trial. Clin Gastroenterol Hepatol. 2015;13(9):1604‐12.e3. doi:10.1016/j.cgh.2015.01.029
- Elli L, Tomba C, Branchi F, et al. Evidence for the Presence of Non-Celiac Gluten Sensitivity in Patients with Functional Gastrointestinal Symptoms: Results from a Multicenter Randomized Double-Blind Placebo-Controlled Gluten Challenge. Nutrients. 2016;8(2):84. Published 2016 Feb 8. doi:10.3390/nu8020084
- Sapone A, Bai JC, Ciacci C, et al. Spectrum of gluten-related disorders: consensus on new nomenclature and classification. BMC Med. 2012;10:13. Published 2012 Feb 7. doi:10.1186/1741-7015-10-13
- Dahlbom I, Olsson M, Forooz NK, Sjöholm AG, Truedsson L, Hansson T. Immunoglobulin G (IgG) anti-tissue transglutaminase antibodies used as markers for IgA-deficient celiac disease patients. Clin Diagn Lab Immunol. 2005;12(2):254‐258. doi:10.1128/CDLI.12.2.254-258.2005
- Catassi, C.; Bai, J.C.; Bonaz, B.; Bouma, G.; Calabrò, A.; Carroccio, A.; Castillejo, G.; Ciacci, C.; Cristofori, F.; Dolinsek, J.; Francavilla, R.; Elli, L.; Green, P.; Holtmeier, W.; Koehler, P.; Koletzko, S.; Meinhold, C.; Sanders, D.; Schumann, M.; Schuppan, D.; Ullrich, R.; Vécsei, A.; Volta, U.; Zevallos, V.; Sapone, A.; Fasano, A. Non-Celiac Gluten Sensitivity: The New Frontier of Gluten Related Disorders. Nutrients 2013, 5, 3839-3853.
- Non-Celiac Gluten Sensitivity Beyond Celiac https://www.beyondceliac.org/celiac-disease/non-celiac-gluten-sensitivity/
- Howdle PD. Gliadin, glutenin or both? The search for the Holy Grail in coeliac disease. Eur J Gastroenterol Hepatol. 2006;18(7):703‐706. doi:10.1097/01.meg.0000221847.09792.34
- Aristo Vojdani and David Perlmutter Differentiation between Celiac Disease, Nonceliac Gluten Sensitivity, and Their Overlapping with Crohn’s Disease: A Case Series Case Reports in Immunology Volume 2013. doi:10.1155/2013/248482
- Pusztai A, Ewen SW, Grant G, et al. Antinutritive effects of wheat-germ agglutinin and other N-acetylglucosamine-specific lectins. Br J Nutr. 1993;70(1):313‐321. doi:10.1079/bjn19930124
- "Cross-Reaction between Gliadin and Different Food and Tissue Antigens" written by Aristo Vojdani, Igal Tarash, published by Food and Nutrition Sciences, Vol.4 No.1, 2013
- Akçay MN, Akçay G. The presence of the antigliadin antibodies in autoimmune thyroid diseases. Hepatogastroenterology. 2003;50 Suppl 2:cclxxix‐cclxxx.
- Hadjivassiliou M, Grünewald RA, Davies-Jones GABGluten sensitivity as a neurological illnessJournal of Neurology, Neurosurgery & Psychiatry 2002;72:560-563.
- Zonulin and Its Regulation of Intestinal Barrier Function: The Biological Door to Inflammation, Autoimmunity, and Cancer Alessio Fasano Physiological Reviews 2011 91:1, 151-175
- Capannolo A, Viscido A, Barkad MA, et al. Non-Celiac Gluten Sensitivity among Patients Perceiving Gluten-Related Symptoms. Digestion. 2015;92(1):8‐13. doi:10.1159/000430090
- Freed DL. Do dietary lectins cause disease?. BMJ. 1999;318(7190):1023‐1024. doi:10.1136/bmj.318.7190.1023
- Cuatrecasas P, Tell GP. Insulin-like activity of concanavalin A and wheat germ agglutinin--direct interactions with insulin receptors. Proc Natl Acad Sci U S A. 1973;70(2):485‐489. doi:10.1073/pnas.70.2.485
- Jönsson, T., Olsson, S., Ahrén, B. et al. Agrarian diet and diseases of affluence – Do evolutionary novel dietary lectins cause leptin resistance?. BMC Endocr Disord 5, 10 (2005). https://doi.org/10.1186/1472-6823-5-10
- J. L. Greger, Nondigestible Carbohydrates and Mineral Bioavailability, The Journal of Nutrition, Volume 129, Issue 7, July 1999, Pages 1434S–1435S, https://doi.org/10.1093/jn/129.7.1434S
- Monica Watrous, Three trends driving gluten-free market Food Business News 2016. https://www.foodbusinessnews.net/articles/7522-three-trends-driving-gluten-free-market
- Miller D. Maybe It’s Not the Gluten. JAMA Intern Med. 2016;176(11):1717–1718. doi:10.1001/jamainternmed.2016.5271
- Mainardi E, Montanelli A, Dotti M, Nano R, Moscato G. Thyroid-related autoantibodies and celiac disease: a role for a gluten-free diet?. J Clin Gastroenterol. 2002;35(3):245‐248. doi:10.1097/00004836-200209000-00009
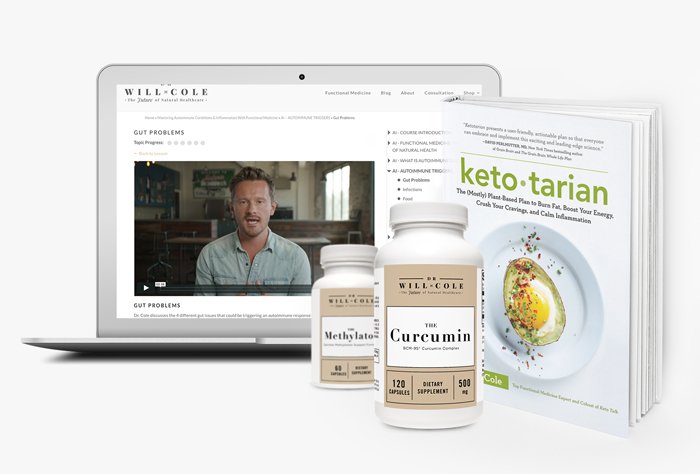
View More At Our Store
Purchase personally curated supplements
and Dr. Will Cole’s books!
The information on this website has not been evaluated by the Food & Drug Administration or any other medical body. We do not aim to diagnose, treat, cure or prevent any illness or disease. Information is shared for educational purposes only. You must consult your doctor before acting on any content on this website, especially if you are pregnant, nursing, taking medication, or have a medical condition.
Our articles may include products that have been independently chosen and recommended by Dr. Will Cole and our editors. If you purchase something mentioned in this article, we may earn a small commission.

BY DR. WILL COLE
Dr. Will Cole, DNM, IFMCP, DC is a leading functional medicine expert who consults people around the globe, starting one of the first functional medicine telehealth centers in the world. Named one of the top 50 functional and integrative doctors in the nation, Dr. Will Cole provides a functional medicine approach for thyroid issues, autoimmune conditions, hormonal imbalances, digestive disorders, and brain problems. He is also the host of the popular The Art of Being Well podcast and the New York Times bestselling author of Intuitive Fasting, Ketotarian, Gut Feelings, and The Inflammation Spectrum.

Gut Feelings
Healing The Shame-Fueled Relationship
Between What You Eat And How You Feel



